Please see letter for appointment details
Please telephone the Endoscopy department on 01234 792269 if this is not convenient for you.
Please contact 07392 126603 If you would like to discuss any aspects of the procedure before your appointment.
If you have not attended a Pre Assessment appointment you will receive a phone call for you to be pre assessed over the phone. This may come through as an unknown number.
Introduction
You have been advised to have a Bronchoscopy to help find the cause of your symptoms. This leaflet may not answer all your questions so if you have any worries please don’t hesitate to ask.
What is a Bronchoscopy?
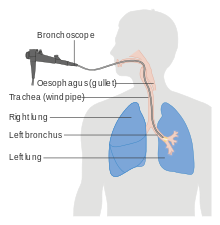
A Bronchoscopy is a procedure, which allows the doctor to examine your airways/breathing tubes of your lungs. The bronchoscopy is done with a thin tube like instrument with a camera on its tip, (called bronchoscope). The bronchoscope enables the doctor to see inside the breathing passages of your lungs and take samples of mucus or tissue from inside your lungs.
Why do I need a Bronchoscopy?
Some of the common reasons why bronchoscopies are done include:
INFECTION
- Specific samples from your lungs can help your doctor to find the causes of infections and give you the appropriate treatment. The doctor can also use the bronchoscope to clear some of the mucus from your breathing passages.
BLEEDING
- The doctor can look inside your breathing passages to determine where the blood is coming from that you are coughing up.
ABNORMAL CHEST X-RAY
- There may be narrowing of a breathing passage or a “spot” on your lungs that the doctor wants to investigate with the bronchoscope and take small samples in order to find the cause.
PERSISTENT COUGH
- Samples taken during a bronchoscopy and an examination of the breathing passages can sometimes help to determine the cause of the cough which is not responding to medication.
NOISY BREATHING
- A bronchoscopy can help to see if narrowing of your breathing passages or erratic movement of your vocal cords (voice box) is causing additional breathing sounds.
Is there an alternative test that I can have instead of a bronchoscopy?
Your doctor can do a breathing test, x-rays and CT scans of your lungs. These tests will give you additional information about your lungs. A bronchoscopy gives very specific information to your doctor by looking inside your breathing passages and obtaining specific samples.
Before your examination
Pre Assessment Appointment
Once you have a booking date you will be pre-assessed over the phone. Please ensure you have contact details of your next of kin, escort and a list of your medicines to hand. The nurse will go into detail about the procedure, check your medical history and answer any questions you may have.
If you are taking Warfarin, Aspirin or any other blood thinning tablet we will advise you at pre-assessment whether you need to stop taking these prior to your procedure.
Before the test you will be asked not to eat anything for six hours.
You may have clear fluids up to 2 hours before your appointment time.
What happens when I arrive?
When you arrive, please book in at reception, you will be then called into the admission area where a nurse will ask you to confirm some details, and go through your medical history and take a set of all relevant observations.
The procedure will be explained to you and you will have the opportunity to ask questions.
The nurse will ensure you understand the procedure and insert a small cannula into the back of your hand or arm. This is where the doctor will administer the sedation and painkiller once you are in the procedure room. You will be asked to sign a consent form by the consultant carrying out the investigation and can ask them any questions prior to having your procedure.
As you will be having sedation you will not be permitted to drive home or use public transport on your own, so you must arrange for someone to collect you from the department and stay with you for 24 hours. The nurse will need to be given their contact details so that they can contact them when you are ready for discharge. Your escort should contact the department on arrival so one of our nurses can take you to them.
What the examination involves?
Once you are in the procedure room the nurse will ask you to lay on the trolley. Once in position you will be given some throat spray to numb the back of your throat (which tastes of bitter bananas) It feels like you can’t swallow, but you can (the back of your throat is just temporarily numb). A sedative and painkiller will be injected into a vein to help you relax. Some patients fall asleep while others feel comfortable and relaxed. Following this sedation, some patients may not remember anything about the test.
The nurses will attach a blood pressure cuff and a clip on your finger (which does not hurt) to measure your oxygen levels. We also routinely give you extra oxygen via a small plastic tube in the nostrils.
When you are lying comfortably and sedated, the scope is placed in the mouth, or nose, past the voice box and into the lungs. You will be able to breathe normally. It does not hurt but there is often coughing which is a normal part of the test. This usually settles down when the local anaesthetic takes effect. The procedure lasts 30 – 40 minutes. We will give you further doses of the sedative as required during the procedure.
The Doctor will look inside the breathing passages and take samples (if required).
Risks
Bronchoscopy is a safe procedure with little risk and complications are relatively rare. There is a small risk of infection and bleeding associated with the procedure, but every effort is made to prevent this from happening.
Air can sometimes leak into the space surrounding your lungs during the procedure but this is not usually a problem and the air can be taken out using a needle and syringe or in some instances a drain (little plastic tube) needs to be inserted and left inside for a couple of hours to drain the air out.
Occasionally patients take a longer time to recover after the procedure and may need to be admitted to hospital for observations.
Sedation
Sedation can occasionally cause problems with breathing, heart rate and blood pressure. If any of these problems do occur, they are normally short lived. Careful monitoring by a fully trained endoscopy nurse ensures that the potential problems can be identified and treated rapidly.
What happens after the bronchoscopy?
As soon as the examination has finished you will be looked after by the nurse in recovery for approximately 2 hours, the nurse will monitor your blood pressure, pulse and oxygen levels. You may require a chest x-ray.
You may cough up small amounts of blood; please inform the nurse if you cough up more than a tablespoon of blood, have chest pain or difficulty breathing.
You should not eat or drink for 2 hours after the procedure. It is common to experience a sore throat, hoarseness and cough after the procedure. In some cases the doctor can give you some initial results of your bronchoscopy but usually you are seen in clinic a few weeks later and the results are discussed with you.
A nurse will go through the discharge information, this includes receiving a clear post procedure leaflet and then you will be escorted to the discharge lounge and given refreshments.
A nurse will take you to the Endoscopy discharge lounge and you will be given refreshments while you wait for your transport home. Once your escort has arrived to collect you from discharge lounge, your escort will need to sign the discharge form, being the responsible adult who will look after you in the next 12-24 hours.
Once home it is important to rest quietly for the remainder of the day. You may resume your normal diet and prescription medication unless otherwise instructed by the doctor.
Going home
The effects of sedation can last for 24 hours so you should not undertake the following for 24 hours following your procedure:
- Drive a car;
- Operate machinery;
- Drink alcohol;
- Sign any legally binding documents;
- Be in charge of any young children.
It is essential if you have had sedation that someone comes into the endoscopy unit to collect you, and stays with you for 12 hours.
Results
These will be given to you at your follow up clinic appointment.
Points to remember:
- If you are unable to keep your appointment please notify the Endoscopy unit as soon as possible
- It is our aim for you to be seen and investigated as soon as possible after your arrival. However the department is busy and your investigation may be delayed. If emergencies occur, these patients will obviously be given priority over less urgent cases.
- The hospital cannot accept any responsibility for the loss or damage of personal property during your time on these premises.
Concerns
If you have any queries regarding the procedure please contact the endoscopy unit between 8am and 6pm Monday to Sunday and the nursing staff will be happy to give you information or advice.
FOLLOWING THIS PROCEDURE YOU MUST NOT DONATE BLOOD FOR 4-6 MONTHS
The reason for this is that your ability to donate blood in the future is dependent upon your diagnosis and the possibility that you might need to undergo further investigations or complete treatments. (British Society of Gastroenterology, 2019)
Additional Information
Having a procedure with a training Endoscopist
Endoscopy Training at Bedford Hospital
Bedford Hospital contributes to the training of Endoscopists and as a result has several trainees working in Endoscopy; this leaflet is provided to inform you about how this may affect your Endoscopy procedure, and support your decision as to whether you are happy to have a trainee perform the procedure.
Although the idea of a trainee may be unnerving it is often a very positive experience. All our Endoscopy trainees are in a structured training programme within the national guidelines.
Around a quarter of Endoscopy lists at Bedford Hospital involve training of Endoscopists.
Will they be supervised?
Under no circumstances are trainee Endoscopists unsupervised. Depending on the experience of the trainee, the experienced Consultant or Senior Nurse Endoscopist will be present, and supervising your Endoscopy procedure throughout or will be immediately available in the endoscopy department. If at any time you or the trainee has any difficulties the trainer can intervene.
All the Endoscopy trainers at Bedford Hospital are accredited Endoscopy trainers and we regularly monitor their training skills.
Is it safe?
We carefully monitor our complication rates for Endoscopy and there is no difference in safety with a trainee Endoscopist.
Will it be more uncomfortable?
We carefully monitor patient comfort and have not found any suggestion it will be more uncomfortable.
Will it take longer?
While learning a trainee may be slower than an independent Endoscopist, however, our trainers are experienced in monitoring the length of a procedure and will take over if procedure seems prolonged. On a training list we allow a longer time for the whole Endoscopy experience, and patients often find this makes for a more relaxed atmosphere.
What should I do if I don’t want a trainee?
If you wish to let us know you are not happy to have a supervised trainee perform your procedure please inform us at least one week in advance of the procedure, so we can ensure you are not booked on a training list. The Endoscopy administrative team are on 01234 792269 or 01234 730567.
