Enhanced Recovery after Bariatric Surgery (ERABS)
Roux-en-Y Gastric Bypass and Gastric Sleeve
‘Major surgery is like running a marathon – both require preparation.’
The aim of this booklet is to provide you with some general information about our Enhanced Recovery After Bariatric Surgery programme (ERABS). It is important that you are aware of what to expect before and after your Bariatric Surgery in terms of how to prepare for your operation and for your recovery.
Enhanced Recovery is a modern, evidence-based approach that can help patients recover more quickly after surgery.
Having an operation can be both physically and emotionally stressful. Enhanced Recovery Programmes try to get you back to full health as quickly as possible.
This booklet is only intended as a guide, as treatment is always planned on an individual basis. Please ask a member of the healthcare team if anything remains unclear, or you have any concerns or questions at pre-assessment, during your stay in hospital or at home.
Research has shown that the earlier a person gets out of bed and starts walking and drinking after having an operation helps to reduce post-operative complications.
Patients and health care professionals are realising the benefits of a shorter stay in hospital, therefore we will work with you in your recovery to keep your stay as short as possible.
You have a very important part to play in your recovery so it is essential to follow the advice that is given to you.
Laparascopic Roux –en-Y gastric bypass
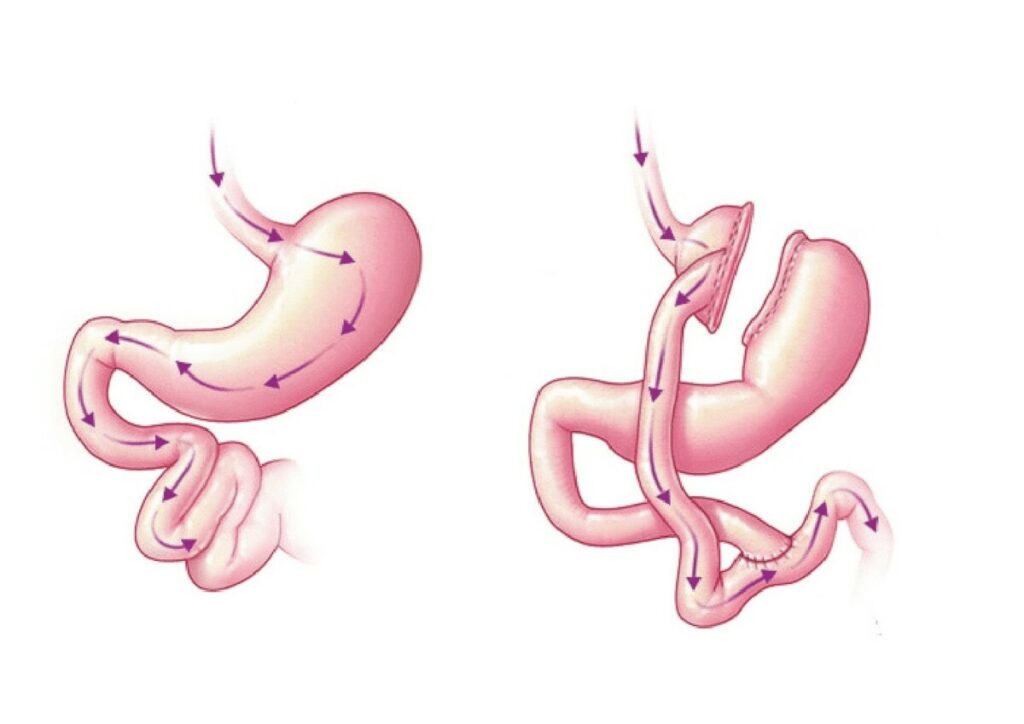 A gastric bypass is where surgical staples are used to create asmall pouch at the top of the stomach.
A gastric bypass is where surgical staples are used to create asmall pouch at the top of the stomach.
The pouch is then connected to your small intestine, missing out (bypassing) the rest of the stomach.
This means it takes less food to make you feel full and you will absorb fewer calories from the food you eat.
Laparascopic Sleeve Gastrectomy
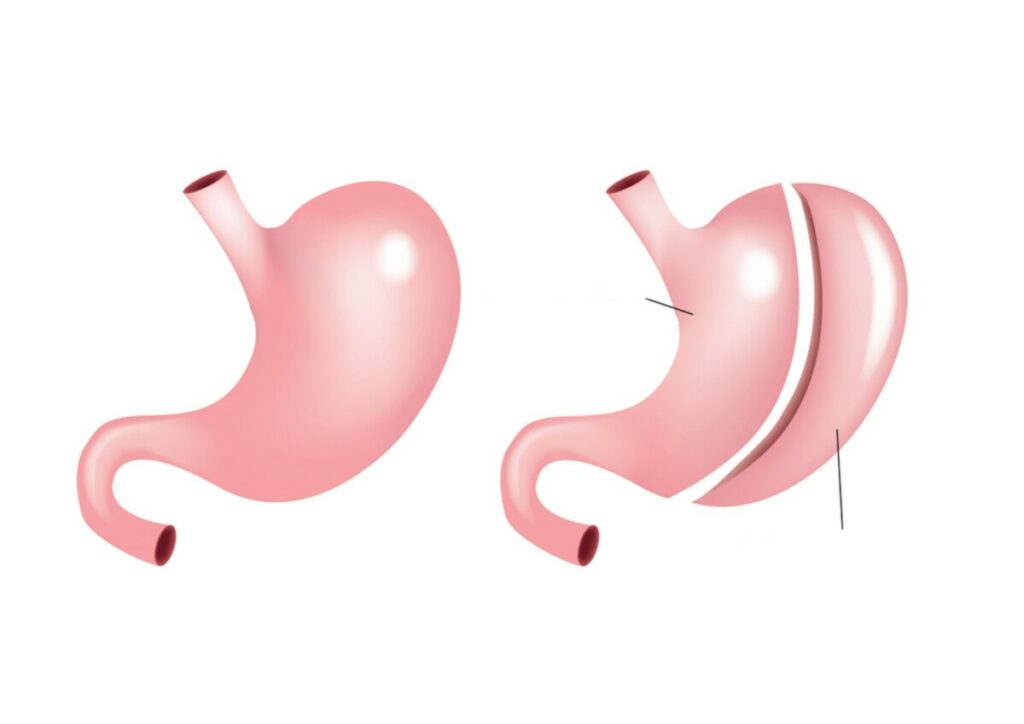
A sleeve gastrectomy is where a large part of the stomach is removed so its much smaller than it was before.
This means you cannot eat as much as you could before surgery and you will feel fuller.
Before your surgery
We expect you to be in hospital for approximately 12 – 24 hours after your surgery – you will be discharged once you have met your discharge criteria which is;
- Drinking fluids adequately (roughly 1.5 litres over 24hrs.
- Pain is reasonably well controlled on the pain medication you are given.
- Nausea reasonably well controlled on anti-sickness medication.
- Medically fit for discharge (surgeons will review and make this decision).
- Please arrive at the hospital as advised in your letter.
- You will be required to fast (stop eating, including no milk) for six hours prior to surgery you can have clear fluids up to 2 hrs before surgery.
- You have been prescribed medications to take prior to the operation. It is extremely important that you take these medications as prescribed and at the right time. If you have any concerns about taking these please contact Obesity Services.
- Any other regular medications that you take should be taken as normal, unless the surgeon or anaesthetist have advised you not to (e.g. aspirin/warfarin are usually stopped before surgery).
- It is very important you follow the low calorie liquid diet for two weeks before surgery. If you can’t drink milk an alternative plan should have been agreed with you. If you have diabetes please monitor your blood glucose and contact the obesity team if they go below 5 or above 9.
Lifestyle improvements
Smoking cessation and limiting alcohol intake
Patients who smoke are at higher risk of complications such as leaks, perforations and stomach ulcers. Therefore we strongly insist that you should quit smoking at least two weeks before your surgery. If you need help with this speak to your GP or your local stop smoking service.
Oral Hygiene
Studies have shown that maintaining good oral hygiene before your surgery can help reduce the risk of some post operative infections. Brushing teeth twice a day is good practice leading up to and after your surgery. If you have any dental concerns we would advise a trip to your dentist and also make them aware of your upcoming surgery.
Increasing exercise
We encourage you to try to increase your level of exercise prior to surgery. Any improvement is good and should be within your own capabilities.
Walking is a great form of exercise which helps boost circulation, builds muscle tone and increases your heart rate which can all help your recovery from surgery.
Any exercise should be continued after surgery but please check with your surgeon before undertaking anything strenuous e.g. lifting, swimming, vacuuming, carrying heavy bags etc to reduce the chance of developing a surgical hernia.
Chair exercises – Sit to stand
These are particularly useful if you have lost muscle mass in your legs or your mobility is poor and you need to strengthen your legs.

Deep breathing exercises
Being able to breathe deeply and comfortably after your surgery is important as this will help to reduce the risk of a chest infection. You should begin to practice these now.
Repeat every hour, 10 times a day!
- Take a big breath in through your nose
- Expand your ribcage as you inhale
- Hold for 3 seconds
- Breathe out slowly through your mouth
- Use a supported cough to clear secretions
- And repeat!
Preparing for your stay in hospital
Prepare for discharge before you come in
When you leave the hospital, you may return to your home or stay with family or friends. You do not necessarily need someone to stay with you if you normally live alone.
Please ensure you have a suitable environment to be discharged to before yo u come into hospital. If you require advice or assistance with this please contact your GP or local Social Services prior to admission .
There are a f ew simple things you will need to do prior to your admission which may make things easier for you when you return home.
- Have a stock of high protein, nourishing fluids ready as listed in Phase 2 of your post op diet.
- Ensure your house is free of clutter so it is easier and safer to move around.
- Changing bed linen is often a good idea.
- Arrange for a repeat prescription of your regular medications (if any).
- Have a supply of paracetamol at home for managing mild pain.
- Please ensure you have transport arrangements for getting home e.g. friends and/or family. If you arrived by hospital transport please ensure you have made arrangements for your return home when booking your admission journey.
- If you need a taxi ensure you have sufficient funds to pay for it.
General Complications
One of the main aims of the Enhanced Recovery Programme is to reduce the risk of complications after surgery. It is important you play an active role in your own recovery to reduce your chances of developing certain complications.
Blood Clots (Deep Vein Thrombosis)
The longer you are in bed or that you are not moving around often after surgery, the greater the risk of blood clots forming. Which is why we encourage you to start circulation exercises in bed when you wake from your surgery and on the ward to get up as soon as possible after the operation only with supervision by a healthcare professional until you are safe on your feet.
Preventative measures include:
- Whilst in bed, do your deep breathing exercises routinely (on page 8)
- Do your circulation exercises:
– Early mobilisation – When you arrive back to the ward you should get up and out of bed once the nurse is happy for you to do so.
– Anti-embolism stockings
– Blood thinning medication
– Drinking fluids as instructed by the nurses and doctors
Chest infections
Everyone is at risk of developing a chest infection after surgery and this risk is increased further if you have chest or lung disease or are a smoker.
Deep breathing exercises are key following abdominal surgery to help get the air right to the bottom of your lungs and therefore can help prevent an infection occurring. Also aiming to be out of bed most of the day is very beneficial.
Nausea and Vomiting
This is one of the main side effects/complications of bariatric surgery.
Usually you will experience some nausea after your surgery and should be given some anti-sickness medication to help control this.
If you are still experiencing nausea or are vomiting and cannot tolerate fluids orally whilst in hospital, please ask your nurse for some anti-sickness medication.
Expect some degree of nausea after you go home, this can be normal. You may require further anti-sickness medications to help with this at home. If you cannot tolerate any fluids or are vomiting you must speak to the obesity team as soon as possible for advice – see the numbers at the back of this booklet.
Pain control following surgery
How is pain assessed?
After surgery, you MUST be able to do the following things comfortably in order to help you recovery quicker;
- Deep breathe
- Cough
- Get in and out of bed
- Walk
You should expect some general discomfort following surgery and on drinking to begin with. This will improve gradually at home. You will be given pain relief by your nurse. If you cannot do any of the above due to pain then you must ask your nurse for some extra pain relief which is called ‘PRN’ or ‘Top up’ this will not be given automatically unless you ask for this.
Pain Score Description
0 (none) No pain at rest or on movement
1-3 (mild) No pain at rest but slight pain on movement
4-7 (moderate) Intermittent pain at rest or moderate pain on movement
8-10 (severe) Continuous pain at rest or severe pain on movement
If you suffer from chronic pain your normal, everyday pain score may already be high so this should be taken into account. If you are on a lot of regular pain medication already then please take as indicated pre-op and ensure you are clear on the instructions post op for any temporary change in dosing. Bring these in with you to hospital and give them to your nurse on arrival to the ward.
Things to bring in with you…
- This booklet!
- A small supply of non-perishable, high protein fluids as per Phase 1 of your diet e.g. OXO cubes, squash, small tubs of custard etc.
- Your CPAP machine – if you use one
- Comfortable day clothes to wear on the ward including footwear
- Nightwear
- Sleep aids e.g. eye masks, ear plugs
- Personal hygiene items (washing, shaving etc.)
- Any medications you are on especially any pain medications as these should be continued after your surgery in most cases and you will be advised by your surgical team. (Please ensure these are in original boxes and that you give them to your nurse on arrival to the ward – do not take any of these unless instructed to by your nurse / doctor).
- Wifi is available throughout the hospital which you can use with your own personal devices, although please be aware, these remain your responsibility.
- Books, magazines personal entertainment devices and a small amount of money if you require anything from the hospital shop.
Admission to Hospital
Day of Surgery
You will receive a letter advising you of your date and time of surgery along with fasting instructions. Please read and follow these carefully. Please note that milk is classed as food and should be stopped 6 hours before your surgery.
- Please ensure you are well hydrated when you come in for your surgery. You should aim to drink between 1.5 – 2 litres of any fluids in the 24 hours before your surgery.
- You will be given a pair of anti-embolism stockings to wear during surgery (unless contra-indicated) which help prevent blood clots forming.
- You will be changed into a hospital gown and you will have to remove or tape any jewellery and remove any dentures and glasses. These can be removed at the last minute if you need them.
- You will be seen by an anaesthetist who will discuss your anaesthetic plan. Please inform them of all the medications and analgesia (if applicable) that you are currently taking.
- Then you will be escorted to theatre by hospital staff.
Day 0 – After your surgery
In the Recovery area
Immediately after your operation you will spend time in the recovery area until a bed space becomes available on the ward.
When fully awake you should begin your deep breathing and circulation exercises in bed and start your fluid intake – unless otherwise indicated by your surgeon.
You should start by drinking approximately 30mls of water (a small medicine cup size) every 10-15 mins – so 4 of these in one hour.
Once you have managed this, you can start to increase the amount you drink and can progress to squash, tea, coffee etc (see page 20 for high protein liquids you can have).
Tepid fluids are best rather than too hot or too cold.
You will be given a Vitamin B12 injection – you will need this every 3 months for life.
On the ward (day 0 until discharge)
You may have some fluids running via a drip in your arm. This will be removed as soon as you are drinking adequately.
You should now get up and move out of bed. Please wait until the nurse checks your blood pressure etc and a staff member should help you do this for the first time. The best time to do this is when you need the toilet.
Getting out of bed and moving around as soon as possible will help to prevent DVTs and chest infections.
Walking also helps get rid of the trapped gas you can have following your surgery which can cause some shoulder tip pain.
If you feel nauseated, please let the nursing staff know so they can give you some anti-sickness medication as soon as possible so you can continue your oral fluids.
It is expected you may have some discomfort following your surgery. You will be given pain relieving medication to help with this. You can also ask for extra pain relief should you require it, it is called PRN or Top Up.
You need to ask your nurse for this as it will not be given automatically.
If you use a CPAP machine at home you should have this with you. You need to use this any time you are asleep after surgery, especially the evening you come back from your surgery.
Short term Discharge Medications
In addition to your life long medications you will be given; Blood thinning injections which reduce the risk of blood clots for 14 days after your surgery.
Lansoprazole fastab helps reduce stomach acid, prevent reflux, indigestion, nausea and promote healing. You should take this for three months.
Senna will help manage constipation whilst on a fluids only diet.
Going Home
This should be the next morning after your surgery providing you have met the discharge criteria which is;
- You are medically fit i.e. your blood pressure, heart rate and temperature are within normal range for you.
- You are drinking adequately (aiming for 1.5 litres over 24 hours)
- Your pain is reasonably well controlled on the pain relieving medication you are on in hospital.
Please ensure you have your transport arrangements made prior to admission. Take any painkillers you are due to have before you set off home as being in a car for a while may be uncomfortable.
If you have travelled some distance then it is sensible to make regular stops to get out and move around and make sure you stay comfortable.
If you have anti-embolism stockings on, these should be worn until your mobility is back to your normal, ensuring you are taking them off for no more than half an hour each day to check, wash and moisturise your skin.
If you are diabetic and on medication, your new medication regime should be explained to you before discharge.
You should avoid flying for 2 weeks after your surgery.
You should not drive until confident and comfortable to do an emergency stop without hesitation. Also, please check with your insurance company.
General Advice for after discharge
In the days and weeks after surgery increasing pain around your tummy, uncontrolled vomiting, being unable to drink, increasing shortness of breath, fever and palpitation may be signs of problems. You should immediately contact us on the number at the back of this booklet.
- Please ensure you understand your medications given to you on discharge.
- Use a small plate or ramekin dish to control your portion sizes.
- Staying well hydrated is important, aim for at least 1.5 litres of fluid per day. Try carrying a bottle of water with you and take frequent sips. Avoid drinking with food as the fluid can fill up your stomach.
- Remember to take all the vitamin and mineral supplements. It takes around six months to adjust to your new diet. If a food does not agree with you then avoid it for a little while and try it again 1-2 months later.
- A meal should take 15-20 minutes to eat. It may take longer to start with, but try not to spend more than 30 minutes at each meal.
- As you move through these stages, you should continue to have your bowels open regularly. You can use senna as needed.
- You should also be passing a normal volume of urine, which should be a pale straw colour. If it is concentrated (dark in colour or strong smelling), contact your Dietitian for advice.
It is important to come to your follow up appointments at 6 weeks, 3 months, 6 months, and 12 months. If you have any concerns about attending the clinic let the bariatric team know to arrange another time for your appointment.
If you cannot commit to this regular follow up you should not consider surgery.
Dumping syndrome
Eating foods and drinks high in sugar or fat can result in the symptoms of ‘Dumping Syndrome’. These might include nausea, sweating, dizziness and diarrhoea. Some people are just more sensitive to this than others. Be especially careful if you are eating out that you select low fat, low sugar foods and drinks.
- You may struggle to find high protein liquids that you can tolerate, especially if you are particularly sensitive to dumping syndrome. Try diluting Complan, Slimfast or other commercial milkshakes with more milk to reduce the sweetness of these drinks. Remember to sip them slowly – a tumbler of fluid should take you an hour to drink.
- Choose low fat, low sugar foods and drinks, have smaller amounts, and remember not to drink with your meals. If you are eating ready meals, have those with less than 5% fat (5g fat per 100g of ready meal).
- If you are having frequent episodes of dumping syndrome, it may be helpful to keep a food diary for a week. This could help you to identify foods/ drinks which are causing you problems.
Phased reintroduction of food
Phase 1: from surgery until Week 3
- When you are fully awake you can begin to drink clear fluids – check first with the recovery staff.
- If you are managing water/clear fluids then you can move onto free fluids. Tea/coffee, milk, clear soup etc progressing to your nourishing high protein fluids
- Drink slowly and regularly.
- Aim for at least 1.5 litres of fluid per day
- On a liquid only diet it is important to ensure that the liquids you choose provide you with enough nourishment and protein to ensure you are not losing muscle mass.
- These nourishing fluids should be your first choice over those with no nutritional value e.g. water.
- You should aim for at least 1.5 litres (3 pints) of fluids per day.
- You will need to take your drinks in small volumes throughout
the day.
Nourishing high protein fluids:
- Semi-skimmed milk
- Condensed soups (made up with milk)
- Smooth yogurt (low fat)
- Complan (made up with milk)
- Slimfast shake
- Sugar free Angel Delight / sugar free Custard
- Yogurt drinks
- Smoothies
- Soya milk (non sweetened) or Oat milk
- Home made soup with lentils beans or chicken (blended)
Other fluids:
- Blended soups
- Water
- Sugar free squash
- Vegetable or fruit juice
- Tea or coffee
- Stock drinks – OXO, Bovril
A typical days intake might be:
Breakfast: 1 glass Complan or Slimfast
Mid morning: 1 glass of milk
Lunch: 1 small cup of soup
1 small pot of smooth yogurt
Mid afternoon: 1 cup of milk
Evening meal: 1cup of Complan or Slimfast
Late snack: 1 glass of milk
Vitamin and mineral supplements:
About 1 week after surgery you should start to take your supplements.
These are the multi vitamin and mineral, the daily iron and calcium supplements, prescribed by your GP You may need to cut these in half, or crush them, and mix with a little yogurt. Please see the table overleaf.
Nutritional supplement, when you should take it, how long for, how much to take and additional information
- Complete 100% A-Z multi vitamin and mineral, Phase 2, for the rest of your life. Forceval or Centrum Chewable 1 each day, Other A-Z 2 each day. Supermarket own brand not advised.
- Calcium supplement e.g.Calceos Or Calcichew-D3Forte OrAdcal –D3, Phase 2, for the rest of your life. To provide 1000 – 1200mg calcium a day. As directed – usually 2 tablets per day. Will be prescribed by your GP.
- Iron Supplement Fersamal Syrup OR Ferrous Sulphate OR Ferrous gluconate OR Ferrous fumarate, Phase 2, for the rest of your life. To provide 60-100mg iron a day 5mls Fersamal syrup per day. 1 x 200 mg ferrous sulphate per day. 2 x 300mg Ferrous gluconate. 1x 210mg ferrous fumarate.
- Vitamin B12 Injection, First dose on ward before discharge, for the rest of your life. 1mg injection every 3 months. Administered by your GP.
Phase 2: Week 3 to Week 6-8 – soft / mashed diet
- You can now begin to introduce soft and mashed foods into your diet.
- You may also find that crunchy foods such as crackers are well tolerated after 6 weeks.
- You may need to blend mince, and other meats, in a blender, to start with.
- A slow cooker, or pressure cooker can be very useful to cook food to the right texture.
- Sauces and gravies are good to make food the right texture.
- If you eat too much food, or you eat too quickly you may experience pain and discomfort. This should ease if you stop eating and rest.
- You may also experience some symptoms of reflux and vomiting, which means that you have eaten too much or have eaten too quickly.
Suitable soft / mashed foods include:
- Lentil or bean soup, blended
- Smooth yogurt
- Soup (with no lumps)
- Cottage cheese
- Eggs, soft cooked
- Low fat cream cheese
- Porridge, Weetabix, Ready Brek
- Crackers with cream cheese, pate, tuna or hummus
- Mashed potato
- Flaky fish in sauce
- Mashed vegetable
- Casseroled meat
- Stewed or tinned fruit
- Minced chicken or meat (blended initially)
- Soya or Quorn mince
A typical dates intake might be:
Early morning: 1 cup of tea, or hot drink
Breakfast: 1 Weetabix with lots of milk
Mid morning: 1 glass of milk
Lunch: Scrambled egg and chopped spaghetti in tomato sauce, stewed or tinned fruit
Mid afternoon: Smooth yogurt
Evening meal: Minced chicken, mashed potato and mashed vegetables
Late snack: Milky drink or pot of custard
Phase 3: Starts at Weeks 6-8
This is the start of your long term eating plan.
- Remember to keep portions small – use a side plate, and a ramekin dish
- Eat regular meals – 3 meals and 1 or 2 snacks is vital
- You can now go back to eating a more solid diet
- Eat foods with high nutritional quality, from all the Food Groups
- If you cannot manage some foods do not give up on them, just try them at a later date.
- Caution foods (which should be tried with care) include non-toasted bread, non-minced red meat, stringy vegetables (green beans, celery), sweetcorn, mushrooms, well cooked rice and pasta, spicy or fried foods, grapefruit and pineapple flesh.
- A hot drink first thing can make it easier to have your breakfast
- We do not advise trying fizzy / carbonated drinks
Starchy foods
Have some at each meal
Choose from these:
- Cereals
- Rice, pasta, potato, cous cous, chapattis
- Toasted bread, crackers
- Tea cakes, breadsticks
Protein foods
Have some of these at each meal these should consist of
around half the food in a meal.
- 1-1 ½ oz ( 30-60g) meat, fish or poultry, or Quorn
- 1 egg
- 2 tablespoons beans or lentils, peanut butter or hummus
Dairy foods
These are also good sources of protein.
- 1 oz ( 30g) hard cheese
- 2 teaspoons soft cheese
- 1 pot yogurt (125g)
Try to choose low fat versions.
Fruit, veg and salad
- A healthy balanced diet has some of these at each meal.
- Aim to have vegetables every day
- Fruit makes a great snack too
- 1-2 portions a day
- Tinned and stewed fruit may be easier to start with
Suggested meal plan:
Hot Drink: Small cup of tea, coffee etc
Breakfast: Weetabix and milk
OR Porridge and fruit juice
OR Toast and peanut butter
Lunch: Lentil soup, or soup and grated cheese, and toast
OR Jacket potato (inside only) and baked beans
OR 1-2 slices wholemeal bread, sliced meat, and cucumber sandwich
OR Crackers and sliced chicken and tomato
Evening Meal: ½ a ready meal (<5% fat or healthy eating) and vegetables
OR Cous cous chicken and vegetable casserole
OR Spaghetti Bolognese and side salad
OR Tuna and tinned sweetcorn pasta bake
Snacks: Yogurt (125g)
OR Fruit – fresh, tinned in juice
OR Custard or rice pudding – low fat versions
OR Crackers and low fat cheese
Frequently Asked Questions (FAQ’s)
Struggling to drink?
You may find it difficult to drink enough fluids. A lot of people feel full after only a few sips. Take a bottle with you wherever you go – sip little & often in between meals.
If you feel pain or pressure on drinking or you experience reflux or vomiting, you may well be drinking too much, too quickly – so slow down!
Constipated?
This may happen for the following reasons– you will be on a liquid diet initially with less fibre; you will be eating and drinking much less and some medication will also slow your bowels down. Try to drink more and gradually build up your daily fluids.
You could have some stewed or tinned fruit every day. Fybogel sachets are not recommended as they swell in the stomach.
Can I start to exercise to help my general fitness?
You should wait until the first follow up with your surgical team (this is approx. 6 weeks post op) before you go to the gym or swimming and until this time you must also avoid any heavy lifting.
It is really important that you gradually build exercise into your life in the long term. You should begin gradually and walking at a good pace is a good place to start. Some sit to stand exercises can be good to strengthen leg muscles and increase your heart rate gently.
When can I start to try to become pregnant?
It is recommended to wait a minimum of 18 months.
Significant weight loss can improve fertility so use your preferred method of contraception during this time.
If you do become pregnant please inform the obesity team and your GP as you will need monitoring more closely and you must attend your follow up appointment. We can provide info on this to your GP / Midwife / Obstetrician.
What happens if I do not take my supplements?
It is essential that you take the iron, calcium and multi-vitamin supplements for the rest of your life as you will no longer naturally absorb these from your diet. If you are struggling to take these for any reason, please discuss this with your Dietitian or GP. Your GP may be able to prescribe alternative supplements.
Why is my poo black and runny?
The iron supplement can affect your bowels and commonly causes dark/black poo and taking a Vitamin C tablet alongside the iron supplement may help. You may also tolerate an alternative iron supplement better, please discuss with your Dietitian and your GP.
What is my expected weight loss?
In the first weeks after your surgery you are likely to experience quite rapid weight loss as you adjust to your new diet and stomach size. Slow, steady weight loss of 1-2 lb (½ – 1 kg) per week is healthy weight loss. Please remember, everyone is different!
Weight loss can slow down and this can be disheartening. Rapid weight loss can lead to muscle loss as well as fat loss. This is one of the reasons why we ask you to ensure your diet contains drinks and foods high in protein – so that you limit the muscle loss as much as possible. It is not healthy to continue to see a rapid weight loss.
You are more likely to keep this off in the long term.
Try to weigh yourself no more than once a week to keep an eye on your weight. It is normal to have weeks where you may not lose any weight, even in the early months post surgery.
Useful Numbers
Non-Urgent Enquiries
Designated Nurse advice line
Monday to Friday, 9am to 4pm
01582 497423
Urgent Enquiries
Obesity Admin Office
Monday to Friday, 8:30am to 4pm
01582 497421
Out of hours and weekend emergencies
Please call the main hospital number 01582 491166 and the operator to connect to the surgical registrar on call and explain that you have had recent bariatric surgery and outline the problem.
