Information for patients
This information sheet answers common questions about jaw joint problems. If you would like further information, or have any particular worries, please do not hesitate to ask your surgeon. In all cases, the surgeon will explain the diagnosis and management techniques to you and answer any questions you may have during the appointment.
What is the temporomandibular joint (TMJ)?
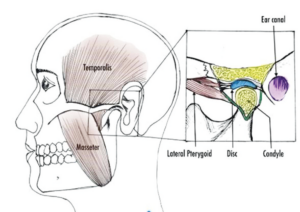
The temporomandibular joint (TMJ) is located in front of the ear between the lower jaw and the skull on both sides of the head. It is the most frequently used joint in the body with primary function of opening and closing of the jaw. The muscles attached to the TMJ help to control the movements of the jaw.
What is temporomandibular disorder (TMD)?
The temporomandibular disorders are a set of conditions which cause pain and dysfunction of the jaw and associated muscles. The symptoms usually resolve spontaneously. In some patients symptoms may be long lasting and hospital treatment may be necessary.
What causes TMD?
Potential causes may include:
- Stress and related habits such as clenching or grinding of the teeth.
- Parafunctional habits like lip chewing, nail biting, chewing gum and any other solid objects.
- Bone disorders such as arthritis.
- Misaligned teeth or imbalanced bite due to loss of teeth.
- Previous trauma to the jaw.
- Certain medical conditions may also lead to TMD.
What are the signs and symptoms of TMD?
- Dull aching pain in front of the ear, radiating to the head, neck and/or cheeks.
- Difficulty opening the mouth wide.
- Locking of the jaw (open or closed position).
- Difficulty chewing food.
- Clicking or crunching sound on mouth opening – on their own are not indicative of disease and do not usually need treatment.
Role of the dentist?
You should see your dentist regularly for assessment of your teeth and gums. Your dentist can give you information regarding your dental health, bite and the replacement or repair of missing, broken or decayed teeth. When any of these factors are altered or disturbed, pain may be increased.
Physiotherapy
Exercises for the jaw can help the surrounding muscles to work better in order to reduce the symptoms. Your GP may be able to refer you for physiotherapy which are helpful in reducing your symptoms.
We recommend some standard exercises which can be performed daily for maximum effect. Using a mirror while doing these exercises can help you maintain good technique.
Jaw exercises
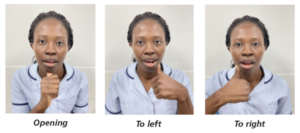
It is important to consciously try and maintain a relaxed jaw position at all times. This is accomplished by having your teeth slightly apart and tongue occupying a position behind your upper front teeth. The following exercises may be done four times (one set). Each set is to be repeated four times a day.
Exercise No. 1
- Place your index finger on both sides of the TMJ
- Touch the roof of the mouth with the tip of your tongue and run the tip as far back as you can towards the soft palate.
- Slowly open your jaw without pulling your tongue away from the soft palate.
- Monitor this jaw opening in a mirror to make sure your opening is a straight line without deviating off to one side.

Exercise No. 2
- Stand and sit in front of the mirror in a relaxed posture in an upright position
- Close your mouth and gently bring your teeth together without clenching
- With the help of a pen, mark a dot or line on the centre point of both your upper and lower lip
- Using a nail file or a piece of card to cover one half of your upper and lower lip so that just your marked dots are visible
- Now very slowly open your mouth making sure the line or dot doesn’t move away or disappear behind the card
- Now close your mouth and repeat the above movement without the line or dot moving.

Exercise No. 3
- Gently place the knuckle of your index finger between top and bottom teeth without biting it too hard.
- Remove the finger and keep the teeth apart in the same position without closing your mouth.
- Gently apply pressure to the jaw with help of your index finger or thumb as shown in the picture.

Exercise No. 4
- Sit in a relax position with back and shoulders straight without tensing up
- Apply anti-inflammatory gel prior to exercise to jaw joints and cheek if instructed to do so
- Position pads of your thumb on upper teeth and index or middle finger on your lower teeth as shown in the photo below
- Gently stretch your mouth with the help of the fingers without actively opening your mouth
- Do it slowly but firmly, it will be uncomfortable but you will feel your jaw joints and cheek stretching. Stretch over for 30-60 seconds
- Hold in this position for 30-60 seconds
- Rest for 60 seconds and repeat steps 1-4 times again.

Other home management techniques to help with TMD
- Avoid eating hard and/or chewy foods
- Avoid chewing gum, nails and any other hard objects
- Hold a heat pack to the painful area
- Apply suitable topical anti-inflammatory gels to the painful areas and gently massage
- Avoid clenching and grinding of the teeth. You can ask your dentist to provide you with a bite guard to help with it
- Avoid opening of the mouth too wide especially on yawning
- Do regular exercises and try relaxation techniques like meditation, yoga or mindfulness
- Improve your posture while sitting or standing.
Surgery
As TMD is self-limiting, conservative management highlighted above helps in relieving your symptoms on most occasions. In some cases surgery may be recommended, especially when the problem is related to the joint itself (mechanical). Your surgeon may request further investigations in the form of blood investigations, MRI and bone scans to understand the problem further.
Surgical options vary in different individuals starting from arthroscopy (direct camera test) and arthrocentesis (washout of joint, open joint surgery or jaw joint replacement which are discussed briefly in this leaflet.
Arthroscopy and Arthrocentesis
The surgical procedure which is done under general anaesthesia can be used for diagnosis and treatment purposes. It is a procedure which is performed under general anaesthesia and involves inserted a small camera in the joint space and performing lysis (reducing stickiness) and lavage (washout) of the jaw joint. Two or three small cuts are made in front of the ear to access the joint.
Additionally, anti-inflammatory medication or your own blood may be injected into the joint. Your own blood may be taken whilst you are asleep which is placed in a machine to form a ‘biological dressing’ called plasma rich fibrin (PRF) or platelet rich plasma (PRP) which may be injected into the joint space. Healing factors in PRF/PRP help in repairing damaged tissue and promoting new growth.
Open joint surgery
This procedure is done under general anaesthesia. It involves making an incision in front of the ear to access the joint. This is usually done to reposition (meniscopexy) or remove damaged disc (meniscectomy) which lies above the joint. Additionally, fat or muscle may be grafted to the site to reduce any scarring (fibrosis) and improve comfort after surgery
Jaw joint replacement
This is the current gold-standard procedure carried out for severely damaged joints where previously described procedures would be ineffective. It is performed under general anaesthesia and involves removing the old joint and replacing it with an artificial (prosthetic) joint.
Living with TMD
TMD can differ from one individual to another. For the majority, TMD may mean occasional pain with or without annoying clicks. In some patients this can be a potentially disabling condition needing medical and/or surgical input. In all cases you should seek specialist opinion through your doctor or dentist.
Online resources
Temporomandibular disorder – NHS
Temporomandibular disorders (TMDs) | Health topics A to Z | CKS | NICE
