Please see letter for appointment details
Please telephone the Endoscopy department on 01234 792269 if this is not convenient for you.
Please contact 07392 126603 if you would like to discuss any aspects of the procedure before your appointment.
If you have not attended a Pre Assessment appointment you will receive a phone call for you to be pre assessed over the phone. This may come through as an unknown number.
Introduction
You have been advised to have an ERCP to help find the cause of your symptoms. This leaflet will explain why ERCP is carried out and what you can expect from the procedure. This leaflet may not answer all your questions so if you have any worries please do not hesitate to ask.
What is an ERCP?
ERCP stands for Endoscopic Retrograde Cholangio Pancreatography. This procedure enables the doctor to examine the common bile duct and the pancreatic duct. ERCP combines the use of X-rays and an endoscope which is a long, flexible tube with a light and a camera on the end.
ERCP is used mostly to diagnose and treat conditions of the bile ducts and pancreas. This will benefit you by providing clear diagnoses.
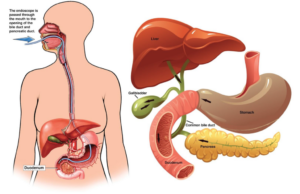
In order to carry out this procedure a tube (endoscope) will be passed through your mouth down into the stomach and the first part of your small bowel (the duodenum) at which point the bile duct and pancreatic duct drain into the small bowel.
What is SpyGlass?
A SpyGlass is a thin endoscope called a cholangioscope that is passed through the duodenoscipe into the bile duct to allow direct vision of the bile duct. The system provides the ability to use specialist equipment to break up and fragment bile of pancreatic duct stones (lithotripsy) using other methods not usually performed during standard ERCP.
It also allows us to sample suspicious areas if there is a concern. Although ERCP is usually an adequate first step to diagnose and treat most bile and pancreatic ducts diseases, SpyGlass is a longer procedure usually done under general anaesthetic, with a higher rise of side effects of complications which your doctor will discuss with you.
Pre Assessment Appointment
You will receive a phone call assessment from an Endoscopy pre assessment nurse before your procedure. Please have to hand a list of your medicines prior to this appointment. The nurse will go into detail about the procedure, check your medical history and answer any questions you might have.
The Preparation
To allow a clear view into your stomach and small intestine (Duodenum) they must be empty, so it is important not to eat for 6 hours before your appointment. You can continue with sips of water up to 2 hours before your appointment time.
One the day of the Procedure
When you arrive at reception you will be asked to take a seat and wait to be called by the nurse who will explain the procedure and go through a series of questions about your general health. You will then be asked to get changed. The Endoscopist will go through a consent form with you and ask you to sign it. This is to ensure you understand the procedure and its implications. If you have any worries or questions do not be afraid to ask. The staff want you to be relaxed as possible for the procedure and will not mind answering your queries. Please tell the nurse or doctor if you have had any reactions to drugs and any allergies you may have. You will need to remove any false teeth or contact lenses. Jewellery or metal objects must also be removed as they interfere with X-rays.
A small cannula will be inserted into a vein in your arm which allows access for the consultant to give you the sedative and any other medications that may be required.
During the Procedure
In the examination room you will be asked to lie on your stomach with you left arm down your side and your right arm up by your head, you will need to turn your head to face the right side. A small clip will be placed on your finger to monitor your pulse rate and oxygen levels during the procedure.
A small sponge will be placed just inside your nose to give you oxygen throughout the procedure and a mouth guard will be placed in your mouth to protect your mouth/teeth.
To ensure that you are relaxed and pain free you will receive a sedative and pain relieving injection which will make you sleepy.
The endoscope will be passed through your mouth down into the stomach and the first part of your small bowel (the duodenum) at which point the bile duct and pancreatic duct drain into the small bowel.
A dye which will show up on the X-rays, is injected via a small tube, passed through the endoscope, into the bile duct and/or the pancreatic duct. Pictures can be taken.
There are then a range of therapies that can be undertaken such as removal of Gall Stones and Stenting. If a narrowing is found, bile can be drained by leaving a short plastic tube (endoprosthesis) in the bile duct.
The dye passes from your body harmlessly.
Results
Before you leave the department, a nurse of doctor will explain the outcome of your procedure and discuss any changes of medication and further investigations or appointments you may require. It is a good idea to have someone with you when you speak to the doctor after the test. Due to the effects of the sedation, many people find they forget everything that has been said to them.
Risks
If an ERCP is carried out purely for diagnosis it carries very little risk. Injection of dye into the pancreatic duct can occasionally cause inflammation of the pancreas known as pancreatitis. The risk of this occurring is approximately 5%.
If the X-rays show a gallstone the doctor will enlarge the opening of the bile duct (Sphincterotomy). This is done with an electrically heated wire (diathermy) which you will not feel. This procedure carries a 1% risk of significant bleeding but this risk is minimised by us checking your blood clotting results before the procedure. If bleeding occurs, you may need a blood transfusion and very occasionally an operation to stop the bleeding.
