Understanding blood clots and how to reduce your risk
Blood clots are also known as venous thromboembolisms (VTEs)
What is a blood clot?
A blood clot in a vein is known as a venous thrombosis. A deep vein thrombosis (DVT) is a clot, which has formed in a deep vein, usually in the leg. It can also occur in other parts of the body. It commonly starts in the calf vein but may extend to the thigh veins.
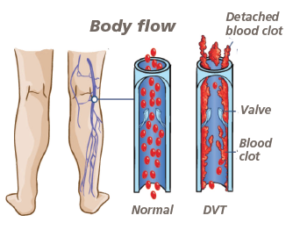
The deep veins of the leg are the larger veins that go through the muscle (not the veins you can see just below the surface) and they carry blood towards the heart. The 3 typical symptoms of DVT are;
- pain
- tenderness
- sometimes swelling associated with skin discolouration
A blood clot can sometimes travel through your veins, moving up the body through to the lungs, blocking an artery. This is called a Pulmonary Embolism (PE), which is serious and life-threatening, requiring urgent treatment.
Risk factors for VTE
- Previous or family history of DVT and / or PE
- Age over 60
- A recent stay in hospital
- Use of oestrogen containing pill
- Dehydration
- Active cancer or cancer treatment
- Significant medical comorbidities
- Major surgery particularly of the pelvis, knees and hips
- Pregnant or have given birth within the last 6 weeks
- Reduced mobility (moving around less than usual for more than 3 days)
- Long distance travel
- Use of hormone replacement pill
- Being overweight or obese
- Varicose veins with phlebitis
- Thrombophilia (a condition where blood clots too easily)
- Some general surgery operations
Reduce the risk of developing blood clots
- Avoid sitting and lying down for long periods of time
- Be active as much as you can whilst in hospital
- Try not to sit with your legs crossed
- Keep hydrated
In the UK, everyone admitted into hospital should be risk assessed for blood clots, and based on this assessment will be offered medication and/or a device to help reduce the risk.
You may be offered compression stockings or intermittent pneumatic compression (IPC) sleeves, which help your blood circulate. IPC sleeves are inflatable worn on your lower legs.
Safe use of compression stockings
Safe:
- Wear them at all times, removing once daily (for no longer than 30 minutes) ideally when washing
- Check correct size and fitting daily
- Inspection hole is under toes
- Ordinary socks and tights can be worn over the top of the compression stockings
- The stockings should cover the end of your toes
Cautions in use:
- Do not use ointments, oils and lanolin-based lotions on your legs as these may damage the stockings
- Do not use if allergic to any of the materials
- Should not be painful
- Should not be too restrictive
- Smooth out any wrinkles/ creases in the stockings
Please speak to your nurse or doctor if your compression stockings or IPC sleeves are uncomfortable or painful or have any other queries or concerns as soon as possible.
When should I stop wearing my compression stockings?
Compression stockings can usually be removed once your mobility is back to your normal level or when your mobility is no longer significantly reduced.
Your doctor or nurse should advise you when you can stop wearing the compression stockings. This will be on the instructions of the nurse or doctor. If you are discharged with embolism stockings please ensure that you are given instructions on their use and when they should be discontinued.
Anticoagulant Medication
You may be offered an anticoagulant medication, which reduces the risk of developing a VTE. These are often given as an injection and may include Tinzaparin, Enoxaparin and Fondaparinux. This is usually injected just under the skin in your stomach or upper leg.
You may develop some bruising around the injection sites, this is common but if you are worried, notice swelling, bleeding or significant bruising please speak to your doctor, pharmacist or nurse.
Some anticoagulant medication in the UK is animal derived. If you have any questions or wish to discuss this further, please speak to your doctor, pharmacist or nurse at the earliest opportunity.
When you leave hospital
Your risk of developing a blood clot will continue for up to 90 days after you are discharged from hospital. You can reduce the risk of developing a VTE by making changes to your lifestyle, such as;
- Stop smoking
- Eat a healthy, well balanced diet
- Take regular exercise and avoid long periods of inactivity including sitting for a long period of time
- Maintain a healthy weight and reduce alcohol intake
- Keep hydrated
- Continue to take mediation as prescribed (if unsure speak to your doctor or pharmacist)
If you are worried about any symptoms you experience, or you have any swelling or pain in your legs or shortness of breath, you must contact your GP immediately.
Further Information
If you have any questions, or would like more information, please contact the doctor, pharmacist or nurse looking after you.
More information about VTEs can be found on NHS Choices website: www.nhs.uk
