What does GDH positive mean?
GDH positive is the abbreviation for ‘Glutamate Dehydrogenase antigen’. This antigen is a substance which can be found in liquid stool (diarrhoea). This substance is typically produced by a bacteria called Clostridioides difficile (C. diff).
A two-stage test to determine if a Clostridioides difficile infection is present is undertaken in the laboratory on liquid stool specimens. The test complies with current guidance as recommended by the department of health.
The first step is to test for the presence of the GDH substance, if found the result is termed as ‘GDH positive’ and it means that you are a carrier of Clostridioides difficile but you do not have an infection of the bacteria.
The second step is to detect the presence of Clostridioides difficile toxin. If that is positive it means that Clostridioides difficile is the likely cause of your diarrhoea.
What does this mean to me?
If you have a GDH positive result, this means that your large bowel is colonised with Clostridioides difficile bacteria but that you do not have the infection.
Clostridioides difficile are bacteria which can be present as part of the ‘normal’ bacteria in the large bowel of up to 5% of healthy adults.
What are the symptoms associated with a GDH positive result?
The majority of patients do not have any symptoms. However one or more of the following may be experienced:
- Watery, foul smelling diarrhoea
- Some patients may develop abdominal pain
- Some patients may develop a temperature
How will I be looked after and prevent the spread of the bacteria?
If you have diarrhoea and your stool has been found to be GDH positive you may be shedding the bacteria to your immediate environment. This exposes other patients to your bacteria and may cause a more serious illness to others. To limit the chance of this happening we nurse you in a side room which can be easily cleaned, more frequently and will either have its own en-suite toilet or a personal commode.
You will be cared for in a single room until your stools have returned to a normal pattern over 48 hours.
Staff caring for you will take precautions by washing their hands with soap and water and wearing apron and gloves to protect you and other patients.
Hands must be washed with soap and water as alcohol hand sanitisers are not effective against the Clostridioides difficile bacteria.
It is important for you to follow rigorous hand hygiene with soap and water too, especially after using the toilet/commode and before eating.
What is the treatment?
Once the diagnoses has been made, your doctor will review your medication and make necessary changes, especially to any antibiotics you may be taking.
You may also receive specific antibiotic treatment for the Clostridioides difficile bacteria.
One of the major adverse effects of antibiotic therapy is that it can cause the production of toxins by the Clostridioides difficile bacteria in patients who are GDH positive, and for this reason doctors need to be extra vigilant when prescribing antibiotics.
What about washing my clothes?
If you have soiled clothing, the nurses looking after you should put it in a plastic bag. Healthy people are unlikely to be affected by Clostridioides difficile. However we do suggest the following actions are taken:
- It is best that the soiled clothing is washed as a separate load to other items.
- The contents of the bag should be emptied straight into the washing machine and the plastic bag put into the rubbish bin.
- Hands should be washed with soap and water at this point.
- A pre-wash can be used if needed to remove excessive soiling.
- The hottest wash that will not damage the clothing should be used.
Will it delay my discharge from hospital?
Your doctors will decide if you are well enough to go home. They may want to make sure that your diarrhoea is settling and that you are able to eat and drink normally.
If you are waiting to be transferred to another hospital, the other hospital will be informed of your GDH positive status.
The doctors looking after you will notify your GP via the electronic discharge letter to make them aware in case your diarrhoea starts again following discharge from hospital.
What happens when I have diarrhoea again?
Sometimes diarrhoea can start again. This may be after you have gone home or while still in the hospital. It is important that you tell a doctor or nurse.
Should I still take antibiotics prescribed by my GP?
Carrying the clostridioides difficile bacteria in your large bowel does mean you are at an increased risk of developing clostridioides difficile diarrhoea compared to someone who doesn’t. This risk is increased if you are prescribed certain medicines (especially antibiotics).
Antibiotics are very important and can be lifesaving so you should not stop them without discussing this first with your GP.
Your GP will make an informed choice involving you in the risks and benefits of the antibiotics and decide whether it is appropriate for you to carry on taking them.
What about visitors?
Your family and friends may still visit but they must clean their hands before and after visiting. They must wash their hands with soap and water. The alcohol sanitiser is ineffective to this bacteria.
Your visitors will be asked to wear appropriate Personal Protective Equipment (PPE), ward staff will advise them and please do not let your visitors sit or lie on your bed.
If your visitors are visiting other patients in the hospital it is advisable that they visit them before visiting you.
Hand hygiene
The role of hand hygiene can help us prevent the spread of infection.
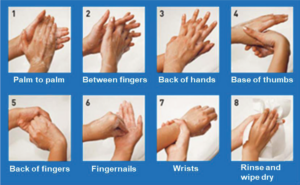
How to wash your hands effectively with soap and water:
- Wet hands thoroughly before applying soap.
- Vigorously rub all surfaces of both hands with soap lather.
- Pay special attention to the finger tips, thumbs and between fingers (these areas are frequently missed when washing hands).
- Rinse off all the soap under running water and dry hands thoroughly.
- Always cover cuts with waterproof plasters.
- When you can, apply hand cream as this helps to prevent dryness and chapping.
Where can I get more information?
If you would like further information please speak to a member of your care staff, who may also contact the Infection Prevention and Control Team for you.
The UK Health Security Agency (UKHSA) website is another source of information:
https://www.gov.uk/government/organisations/uk-healthsecurity-agency
Infection Prevention and Control contact details
You can contact the team Monday – Friday between 9am – 5pm on the following numbers:
Bedford
01234 795848
Luton
01582 497321
