Caring for a residual limb
General Care for your Residual Limb (Amputated side)
Your residual limb needs care to enable you to be as mobile as possible. Problems occurring to your skin over your residual limb may mean that you are unable to wear your prosthesis for a while, so by using simple care techniques, this situation can be avoided.
Always consult your Nurse or Prosthetist if you notice sores or blisters on your residual limb. If ignored, these minor problems can turn into serious infections.
CLEANLINESS
- Always remember that your residual limb will be encased in a complete or partially complete airtight socket that does not breathe or allow perspiration to evaporate.
- Perspiration is acidic and salty and if allowed to dry it forms tiny crystals similar to sandpaper on your skin. If left on your skin inside the socket, bacteria can grow, your skin can become broken and infections may occur – hence the need for cleanliness.
Daily Care
- Your residual limb should be washed with a mild soap, then rinsed and dried with a clean towel. Do not use talcum powder or alcohol spirits on the skin.
- At night apply a moisturising cream such as E45. Moisturiser should only be applied after wearing your prosthesis, not before.
- If you are prone to perspire/sweat you may need to wash your residual limb more than once per day, always ensuring you dry thoroughly prior to wearing your prosthesis.
- Aluminium based anti-perspirants such as Odaban, Anhydrol Forte, or Driclor may be of benefit (please speak to our Doctor)
Moist or damp skin can quickly rub and become sore
- All materials that come in contact with your skin (stump socks, nylon sheaths etc) should be washed daily with mild detergent and rinsed well. Silicone liners should be washed as per the manufacturer’s instructions or advice given to you by your Prosthetist.
- Do not shave your residual limb as this may lead to ingrown hairs, which often leads to infected hair follicles.
Inspection of your Limb
When you remove your prosthesis, always inspect your residual limb noting any rubs or sore places. This is very important if you are a diabetic or have reduced sensation and a reduced blood supply.
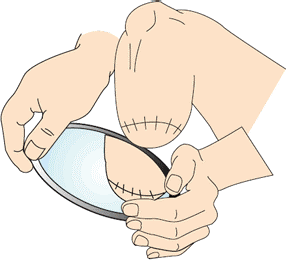
If necessary, use a mirror or ask someone to help you:
If you do find a sore or blister on your residual limb, gently clean the area and apply a dry dressing. Then, contact the Limb Fitting Centre and report your problem so you can be seen to as soon as possible by the appropriate members of staff. If you cannot attend quickly, seek help from your GP and avoid wearing your limb.
Touch and Desensitisation
Many amputees experience sensitive residual limbs or hypersensitivity of the effected limb around scar areas or muscles. This often results in increased discomfort and pain that can affect the use and function of the residual limb.
Ask your therapist to talk through the application of touch and pressure to the soft tissues of the residual limb. Desensitisation can be a highly effective method of reducing the sensitivity of the nerves and underlying tissues, therefore reducing the associated pain and discomfort. This involves rubbing, and tapping the end of your residual limb using different materials.
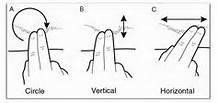
Begin with a light, gentle touch with cotton wool in a circular motion.
When you are able to tolerate this pressure, progress to a rougher material such as paper towel.
Finally, advance to a terry cloth towel as this is the same type of material you are likely to use with your prosthesis.
Stump Massage and Scar Mobilisation
Stump massage is a technique which helps to prevent your skin from sticking to (or adhering to) the cut end of bone which helps improve the comfort of your prosthesis and reduce the risk of blistering.
Stump massage is best performed when applying moisturising cream. Using your hands, gently knead your stump in a circular fashion along the scar line and over the end of the stump. Try the techniques below on the scar line itself:
In time, increase the massage pressure over your stump as tolerated. You may be required to continue with stump massage for several months or, until your scar moves freely over the underlying tissue.
This technique will help keep your skin mobile, reduce the risk of skin breakdown and socket discomfort in the future.
