This information leaflet is for patients who are having an examination known as an ERCP. The leaflet explains the reasons for examination, what is involved and any possible risks or side effects.
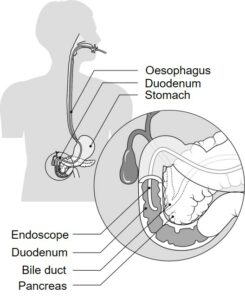
An ERCP (endoscopic retrograde cholangiopancreatography) is an examination of the stomach, duodenum, pancreas and bile ducts. A long thin flexible tube called a duodenoscope is passed through the mouth into the stomach and the duodenum. An image is then projected onto a screen enabling the Endoscopist to examine the area and to introduce a liquid dye into the bile ducts and/or pancreatic ducts so they can be seen on x-ray pictures.
Reasons for having an ERCP
- Treatment – stones in the bile duct can be removed after enlarging the opening from the bile duct into the duodenum. In the bile ducts, narrow areas and obstructions can be bypassed if necessary by placing a small plastic/metal tube (a stent) across the narrowing.
Preparation
Before the test you will have had blood tests taken and we also ask that you let us know in advance if you are allergic to anything.
For the examination to be successful your stomach must be empty, so it is important that you have no food for six hours before the examination and water only up until two hours before.
If you have diabetes, or you are taking anticoagulants (blood thinning medication) such as warfarin, dabigatran, rivaroxaban, edoxaban or apixaban, and/or antiplatelet medication such as ticagrelor or clopidogrel you will be given specific instructions in advance.
Please read and complete your medical assessment form in advance of your procedure. You will also be sent a consent form which a nurse will discuss with you on the day.
If you have any concerns about the test, please speak to the doctor or nurse. On the day, please bring any tablets or medicines which you are currently taking.
On arrival at the hospital
- Please go to the admissions desk at the main reception. They will direct you to the arrivals lounge or to your ward
- Your doctor will explain the examination and ask you to sign a consent form to confirm that you understand the procedure and agree to go ahead with it
- You will be given a hospital gown to wear and an identity band, which you should check for accuracy
- Before the examination you will need to remove any dentures, glasses, contact lenses or jewellery. We recommend that you leave any valuables at home
The examination
Your examination will take place in the X-ray department and will begin with an anaesthetic spray used to numb the back of your throat.
You will be given an injection of sedative and painkiller to make you relaxed. Sedation may also make you feel sleepy but for most patients it induces sleep after the examination, rather than during it.
The test will start with you lying on your left side on a couch and oxygen will be provided to you via a soft tube placed in your nostrils and a mouth guard added to protect your teeth.. The doctor will gently insert the duodenoscope through your mouth into the stomach and duodenum. This will not make your breathing or swallowing difficult.
The doctor will pass some air into the intestine so the duodenum can be clearly seen. Most of this air will be sucked out at the end of the test.
During the test a liquid will be injected into the bile duct and/or pancreatic duct. X-ray pictures will also be taken as appropriate.
If a blockage or stones are found in the bile duct, the endoscopist will try to treat the blockage or remove the stones. In total, the examination should take between 15 to 60 minutes, after which the duodenoscope will be quickly and easily removed.
After the examination
After the procedure you may be able to return home the same day providing you have a chaperone for 24 hours. However, there are some circumstances where you may be required to stay in hospital overnight.
Following your examination you will be given a suppository (indomethacin), provided you are not allergic to NSAIDs (e.g. ibuprofen or aspirin), and 1 litre of intravenous (through the vein) over 4-6 hours, as this has been reported to reduce the risk of pancreatitis. You will then be taken back to the endoscopy recovery area where you will be able to recover before going home.
You may eat and drink as soon as you feel you can swallow normally, depending on your doctor’s instructions. At first you may feel a little bloated from some air left in your stomach – this will pass and you should not need to take any medicine for it.
Subsequently, you will be informed of the result of the investigation and advised, if necessary, should further treatment be required.
The sedative effects (if administered), may make you sleepy and can last for 24 hours. Even though you may feel alert you must be accompanied home. If you had the sedative injection and/or analgesia, you must have a responsible friend or relative to take you home and stay with you for 24 hours. If this is a problem, please telephone the department as soon as possible.
For 24 hours post procedure you must not drive a car, drink any alcohol, sign any legally binding documents, look after any dependents or operate machinery.
You should continue to take your normal medications unless we advise otherwise. If you were asked to stop any medicines before your procedure we will confirm when you can restart them before you leave.
Risks and complications
While the vast majority of people who undergo ERCP have no serious complications, like any procedure there are some risks. For an ERCP there is a risk of having one of the following complications:
- Inflammation (acute pancreatitis) – occasionally the pancreas can become inflamed due to the special x-ray dye (there is a less than 5% chance that this will happen*). If it occurs you will need to stay in hospital for a few days to allow it to settle down.
- Internal bleeding (less than 2%*) – this may occur if the doctor has to widen the opening to the bile duct. It usually stops after a short time but very occasionally requires a blood transfusion or further treatment.
- Perforation (less than 2%*) – a small tear in the intestine, which can happen during the procedure. This is rare and may not need treating at all but you might have to stay in hospital so the tear can be repaired surgically.
- Failure to complete the procedure (less than 15%*)
- Mortality (less than 1%*)
If you have any concerns about the risks, please discuss them with your specialist before the test.
*JAG Accreditation Programme – Guide to Meeting Quality and Safety Standards (November 2019)
What are the alternatives to ERCP?
The bile ducts and the pancreas can be investigated with various scans for diagnostic purposes, however they cannot be treated at the same time.
Blood Donation
Following this procedure, you must not donate blood for 4-6 months. The reason for this is that your ability to donate blood in the future is dependent upon your diagnosis and the possibility that you might need to undergo further investigations or complete treatments (British Society of Gastroenterology Guidance; updated February 2020).
Air travel
You should not undertake any air travel for 2 weeks after your procedure.
Sleep Apnoea
Please bring your CPAP machine with you for your appointment as due to the possible side effects of the sedative injection/ pain relief injection it might be necessary for it to be used to ensure your safety.
Pacemaker Device or Implantable Cardioverter Defibrillator (ICD)
Please bring your pacemaker device or implantable cardioverter defibrillator manufacture information card with you as the cardiac technician will need that information to make sure your device is safe for you during this procedure.
Medication
Please do not stop taking any prescribed medication prior to the procedure, unless you have been advised by the doctor, including blood pressure tablets.
Having a procedure with a training Endoscopist
There are no trainees for ERCP at the L & D site.
For further information
For any medication queries please telephone 07815 178 199
Mon-Sat between 10:30-11:30am and 14:30-15:30pm only.
Outside of these hours, this telephone is for Emergency calls only.
