Having a Flexible Sigmoidoscopy
This information leaflet is for patients who are having an examination of the lower bowel (known as a flexible sigmoidoscopy). It explains the reasons for the examination, what is involved and any possible risks or side effects.
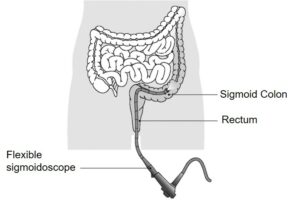
A flexible sigmoidoscopy is an examination of the left side of the large bowel (the colon) using a flexible instrument called a colonoscope. This is introduced into the colon via the back passage and projects an image which is displayed onto a screen.
Reasons for having this examination
- Diagnostic – so the doctor or nurse specialist can see any abnormalities.
- Investigative – to take samples from the lining of the bowel (biopsies) for further tests in the laboratory.
- Treatment – so abnormalities such as polyps (small bumps in the bowel lining) can be removed
- Surveillance – to re-examine any previous problems
Preparation for the examination
- For this examination to be successful your bowel must be as empty as possible. On the day before the test we ask that you follow a low-residue diet (examples of which are shown in this leaflet).
- In order to clear your lower bowel before the examination, you will have an enema. You can do this yourself at home and we advise you to do so, in order to maximise your comfort during the process. Information on giving yourself an enema at home is available on pages 11.
- In exceptional circumstances, enemas can be given when you come to the endoscopy unit, however this is likely to delay your procedure and discharge.
- Occasionally a more thorough preparation is needed with laxatives. Should this be required it will begin the day before your examination and you will be given the necessary instructions.
- You should not eat or drink anything for two hours before your appointment.
- Patients must not stop any prescribed medication including blood pressure tablets unless advised by your consultant. If you are however on any iron preparations or medication that may make you constipated, this must be stopped 7-10 days before your procedure.
- The procedure can be performed if you are taking blood thinning medication such as Warfarin, clopidogrel, ticagrelor, dabigatran, rivaroxaban, edoxaban or apixaban as long as you tell us that you are taking them. If this is the case you may be asked to have a blood test to check your blood clotting, the day before the procedure. Occasionally, these may need to be stopped; your referring consultant will have advised you with regards to this.
- Please read and complete your medical assessment form in advance of your procedure. You will also be sent a consent form which a nurse will discuss with you on the day.
- Please also bring a dressing gown and slippers with you.
If you have not been advised what to do about your medicines or if you require any additional access or support, please telephone 07815 178199.
Mon- Sat between 10:30 – 11:30am and 14:30 – 15:30pm only.
Outside of these hours, this telephone is for Emergency calls.
On arrival at the hospital
- Please go straight to the Endoscopy Unit and ring the bell to let the staff know you have arrived.
- Procedure times can be unpredictable so you may have to wait a while, it is a good idea to bring something to read.
- A nurse will discuss your medical history with you, while also checking your pulse, blood pressure, oxygen levels, blood sugar (if diabetic) and clotting (if on anticoagulants). They will ask any necessary additional questions and you will have the opportunity to ask anything you may want to know.
- The nurse will go through the consent form with you to confirm that you understand the procedure and agree to go ahead with it, after which you should sign the form. You will be given an identity band which you should also check for accuracy.
- If you have not already had the enema at home, this will now be given to you.
- You will then be asked to change into a hospital gown. Put on your dressing gown over this and wait until you are taken through to the examination room.
- A nurse will remain with you throughout the examination.
The examination
During the examination you will lie comfortably on your left side on a couch. The doctor or nurse specialist will gently pass the flexible tube into your large bowel via the back passage and some air will be passed into your bowel to expand it for a clear view. This may cause some discomfort but it will not last.
You may feel as if you want to go to the toilet but be reassured that this will not happen. Most of the air will be sucked out at the end of the test.
A biopsy (a small sample of tissue from the bowel lining) may be taken during the examination to be sent to the laboratory for further tests. This does not cause pain.
Occasionally polyps are found in the bowel and can be removed. This again is painless but can result in bleeding from the lining of the bowel when the polyp has been removed. This bleeding usually settles down quickly.
The examination usually takes between 10 – 20 minutes. If you experience abdominal pain you may be offered Nitrous Oxide gas to relieve it if you have previously agreed to its use. The effects of the gas wear off quickly but you will not be allowed to drive for 45 minutes after the procedure.
Sedation is not usually given for this examination; however you can discuss this with your doctor if you feel you need it. If you decide that you need sedation you must have a friend or relative to take you home and stay with you for 24 hours. You will not be allowed to drive or use machinery in that time.
After the examination
Following the examination you will be able to get dressed and will be offered refreshments. If you had sedation, you will rest in the unit beforehand.
The nurse will tell you the result of the examination before you go home and you will be given a copy of your examination report.
You will be told what further tests or treatment if any is needed, however any biopsy results will take longer and will be sent to your GP.
After your examination you may still have wind. This will pass and you do not need to take any medication for it.
Individuals are unable to donate blood for 4-6 months following any endoscopic procedure. (British Society of Gastroenterology guidance; updated February 2020).
Going home
As soon as you feel ready you may go home and resume your normal diet and activities unless you were given sedation or Nitrous Oxide gas, in which case you must wait as previously outlined in this leaflet.
What are the risks?
Flexible sigmoidoscopy is a safe examination for most people. Serious problems are rare, but life threatening complication are possible. However, you need to weigh up the benefits against the risks of having the procedure. there can be risks from having the examination itself, as well as from the sedation. the main risks are;
- A tear (perforation) in the lining of the bowel: Nationally this happens to approximately 1 in 1000 people. The risk of a tear is higher with polyp removal. If we know before your procedure that you have a large or difficult to remove polyp, your endoscopist will discuss the risks with you in more detail. An operation may be required to repair a tear if it cannot be closed during the flexible sigmoidoscopy.
- Risk of a missed lesion: Although flexible sigmoidoscopy has been selected as the best test to diagnose your symptoms, no test is perfect. There is a risk of 1 in 100 that we might miss a large polyp or other important finding during your test.
- Bleeding where we take a sample (biopsy) or have removed a polyp: Happens to about 1 in 100 people, but this is usually minor and often stops on its own.
- Short term problems with breathing, heart rate and blood pressure ( related to sedation): 1 in 100. We will monitor you carefully so that if any problems do occur they can be treated quickly. Older people and those with significant health problems (for example, people with serious breathing difficulties) may be at higher risk.
- Heart attack or Stroke (related to sedation): 1 in 5000
Women taking the oral contraceptive pill should be aware that taking bowel preparation might prevent absorption of the pill. Additional contraceptive precautions should be taken until the next period begins.
If you have any concerns about these risks, please speak to the endoscopy staff before the examination.
Are there any alternative procedures?
Barium x-rays and scan can image the lower bowel but are not as accurate as a flexible sigmoidoscopy. Biopsies cannot be taken and procedures cannot be performed with x-rays and scans.
Air travel
If you have undergone a therapeutic procedure, you should not undertake any air travel for 2 weeks after your procedure. You will be advised on discharge which procedure you have had.
Sleep Apnoea
Please bring your CPAP machine with you for your appointment as if you choose to have a sedative injection it might be necessary for it to be used to ensure your safety.
Pacemaker Device or Implantable Cardioverter Defibrillator (ICD)
Please bring your pacemaker device or implantable cardioverter defibrillator manufacture information card with you because a cardiac technician might be required to check your device and will need that information to make sure your device is safe for you during this procedure.
Some suggestions for low residue meals
Breakfast
- Cornflakes or Rice Krispies with milk
- White bread, butter or low fat spread, jam without seeds, or rindless marmalade
- Boiled egg on white toast
Lunch
- White bread sandwich with low fat spread or butter with fillings of cheese, ham or tuna with seedless mustard
- Clear soup with white bread
Dinner
- Plain pasta
- Chicken or any grilled meat
- White rice, poached fish
- Egg and bacon quiche
- Mashed, boiled, chipped or roast potatoes
Patient Information
Administering a phosphate enema at home
- You will need to have an enema to clear the lower bowel. This can be given in the privacy and comfort of your own home, before attending the endoscopy unit for the examination
- Giving your enema at home allows you to take your time, which will result in better bowel preparation for the flexible sigmoidoscopy
- A rectal phosphate enema can be purchased from your local chemist/pharmacy
Information Information
We have designed this information leaflet to simplify the manufacture’s instructions. Please follow our instructions carefully
What is your medicine used for?
To ensure that the bowel is empty. This will then allow us to view the lining of the bowel during your flexible sigmoidoscopy.
Side effects of the phosphate enema
You may experience stomach cramps, dizziness or feel clammy. If this happens try lying on your bed or have a cup of tea. Once you have been to the toilet the stomach cramps should pass.
What to do the day before your appointment
The day before your appointment, please take a low-residue diet. You may resume your usual diet after your flexible sigmoidoscopy.
On the day of your appointment
Two hours before you leave for your appointment do not have any more to eat or drink and please follow these instructions:
- Place a thick towel on the bed for you to lie on
- Remove the tip from the nozzle of the enema
- Lay on your left-hand side on the towel with your knees bent
- Slip the nozzle end gently into your bottom. Do not use force. Squeeze the contents until the bottle is empty and then remove the nozzle. You may dispose of the bottle in the normal household waste
- Try to hold the fluid in your bowel for as long as possible; ideally 10-15 minutes
- When you need to empty your bowel, you can get up to sit on the toilet. You may need to do this 2-3 times to completely empty your bowel
- If the bowel preparation delays your arrival, please telephone the endoscopy unit
- If you are unable to administer the enema yourself please inform the staff in the endoscopy unit and it will be administered prior to your procedure
Having a procedure with a training Endoscopist
Endoscopy Training at Luton and Dunstable Hospital
Luton and Dunstable Hospital contributes to the training of endoscopists and as a result has several trainees working in Endoscopy; this leaflet is provided to inform you about how this may affect your Endoscopy procedure, and support your decision as to whether you are happy to have a trainee perform the procedure.
Although the idea of a trainee may be unnerving it is often a very positive experience. All our Endoscopy trainees are in a structured training programme within the national guidelines.
Will they be supervised?
Under no circumstances are trainee Endoscopists unsupervised. Depending on the experience of the trainee, an experienced Consultant will be present, and supervising your Endoscopy procedure throughout or will be immediately available in the Endoscopy department. If at any time you or the trainee has any difficulties the trainer can intervene. All the Endoscopy trainers at Luton and Dunstable Hospital are accredited Endoscopy trainers and we regularly monitor their training skills.
Is it safe?
We carefully monitor our complication rates for Endoscopy and there is no difference in safety with a trainee Endoscopist.
Will it be more uncomfortable?
We carefully monitor patient comfort and have not found any suggestion it will be more uncomfortable.
Will it take longer?
While learning a trainee may be slower than an independent Endoscopist, however, our trainers are experienced in monitoring the length of a procedure and will take over if procedure seems prolonged. On a training list we allow a longer time for the whole Endoscopy experience, and patients often find this makes for a more relaxed atmosphere.
What should I do if I don’t want a trainee?
If you wish to let us know you are not happy to have a supervised trainee perform your procedure please inform us at least one week in advance of the procedure, so we can ensure you are not booked on a training list. The Endoscopy Booking Office can be contacted on 01582 497273.
For further information
For any medication queries please telephone 07815 178199
Mon – Sat between 10:30 – 11:30am and 14:30 – 15:30pm only.
Outside of these hours, this telephone is for Emergency calls only.
