Introduction
You have been advised to have a Bronchoscopy to help find the cause of your symptoms. This leaflet may not answer all your questions so if you have any worries please don’t hesitate to ask.
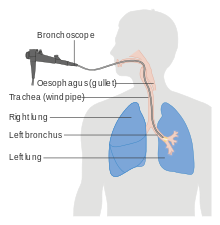
What is a Bronchoscopy?
A Bronchoscopy is a procedure, which allows the doctor to examine your airways/breathing tubes of your lungs. The bronchoscopy is done with a thin tube like instrument with a camera on its tip, (called bronchoscope). The bronchoscope enables the doctor to see inside the breathing passages of your lungs and take samples of mucus or tissue from inside your lungs.
Why do I need a Bronchoscopy?
Some of the common reasons why bronchoscopies are done include:
INFECTION
- Specific samples from your lungs can help your doctor to find the causes of infections and give you the appropriate treatment. The doctor can also use the bronchoscope to clear some of the mucus from your breathing passages.
BLEEDING
- The doctor can look inside your breathing passages to determine where the blood is coming from that you are coughing up.
ABNORMAL CHEST X-RAY
- There may be narrowing of a breathing passage or a “spot” on your lungs that the doctor wants to investigate with the bronchoscope and take small samples in order to find the cause.
PERSISTENT COUGH
- Samples taken during a bronchoscopy and an examination of the breathing passages can sometimes help to determine the cause of the cough which is not responding to medication.
NOISY BREATHING
- A bronchoscopy can help to see if narrowing of your breathing passages or erratic movement of your vocal cords (voice box) is causing additional breathing sounds.
Before the test you will be asked not to eat anything for six hours. You may have clear fluids up to 2 hours before your appointment time.
Advice on Medication:
The nurses from the ward will make sure to withhold your medication if you are taking blood thinning.
A sliding scale maybe prescribed if you have diabetes Type II on insulin. The ward nurses can arranged this for you.
What the examination involves?
Once you are in the procedure room the nurse will ask you to lay on the trolley. Once in position you will be given some throat spray to numb the back of your throat (which tastes of bitter bananas) It feels like you can’t swallow, but you can (the back of your throat is just temporarily numb). A sedative and painkiller will be injected into a vein to help you relax. Some patients fall asleep while others feel comfortable and relaxed. Following this sedation, some patients may not remember anything about the test.
The nurses will attach a blood pressure cuff and a clip on your finger (which does not hurt) to measure your oxygen levels. We also routinely give you extra oxygen via a small plastic tube in the nostrils.
When you are lying comfortably and sedated, the scope is placed in the mouth, or nose, past the voice box and into the lungs. You will be able to breathe normally. It does not hurt but there is often coughing which is a normal part of the test. This usually settles down when the local anaesthetic takes effect. The procedure lasts 30 – 40 minutes. We will give you further doses of the sedative as required during the procedure.
The doctor will look inside the breathing passages and take samples (if required).
Risks
Bronchoscopy is a safe procedure with little risk and complications are relatively rare. There is a small risk of infection and bleeding associated with the procedure, but every effort is made to prevent this from happening.
Air can sometimes leak into the space surrounding your lungs during the procedure but this is not usually a problem and the air can be taken out using a needle and syringe or in some instances a drain (little plastic tube) needs to be inserted and left inside for a couple of hours to drain the air out.
Occasionally patients take a longer time to recover after the procedure and may need to be admitted to hospital for observations.
Sedation
Sedation can occasionally cause problems with breathing, heart rate and blood pressure. If any of these problems do occur, they are normally short lived. Careful monitoring by a fully trained endoscopy nurse ensures that the potential problems can be identified and treated rapidly
When will I go back to the Ward?
As soon as the examination has finished you will be looked after by the nurse in recovery to monitor your blood pressure, pulse and oxygen levels. The nurse from the ward will come to take you back and you will be monitored in the ward. You may require a chest x-ray if required the ward doctor and nurses can arrange this for you.
You may cough up small amounts of blood; please inform the nurse if you cough up more than a tablespoon of blood, have chest pain or difficulty breathing.
You should not eat or drink for 2 hours after the procedure.
It is common to experience a sore throat, hoarseness and cough after the procedure.
A nurse/doctor from the ward will go through the result of your procedure
