Inpatient Induction of Labour
Patient relatives and carers information booklet
Your name:
EDD:
Indication for induction:
Date induction booked for: (if applicable)
Induction discussed by:
Date of discussion:
To translate this leaflet, click on the ‘Show Accessibility Toolbar’
![]()
Then click on the translate button

Making decisions about your care
The BRAIN tool helps you ask the right questions and have better conversations, so you can make the best decision for you and your baby.
Benefits
- What are the benefits of an induction of labour?
Risks
- What are the risks of an induction of labour?
- Are there any specific side effects that would be personal to you?
Alternatives
What are the alternatives to an induction of labour?
Intuition
- How do I feel about the idea of an induction of labour?
Nothing
- What if I do nothing/ wait and see?
- What happens next?
You don’t have to make a decision straight away; you can take some time to decide the best course of action for you.
Your doctor or midwife will explain why they are recommending or offering an induction of labour, but it is your choice whether to go ahead with an induction.
What is induction of labour?
Labour is a natural process that usually starts on its own between 37 and 42 weeks of pregnancy. During pregnancy your baby is surrounded by amniotic fluid (your waters). Before or during labour, this sac of amniotic fluid ruptures (your waters breaking).
Toward the end of pregnancy, the cervix (opening to the womb) softens and shortens. This is called ‘ripening of the cervix.’
This process can occur over days or weeks. During labour, your cervix dilates (opens) and your uterus contracts to push your baby down and out.
Induction of labour is a medical procedure intended to start the labour artificially. You may be offered an induction if you or your baby have a condition that means it will be safer to have your baby sooner. Induction will usually be planned in advance.
You will be able to discuss the risk and benefits with your doctor or midwife and decide if induction is the right choice for you.
The risks and benefits of induction, watching and waiting, or a planned caesarean will depend on the reason you’re being offered induction and your own personal circumstances. On average, labour is induced in 3 – 4 out of 10 pregnancies nationwide and our rates are similar.
The most common reasons for induction
- To reduce the risk of stillbirth if your pregnancy is lasting longer than 41 weeks (we recommend induction between 41 and 42 weeks).
- To reduce the risk of infection if your waters have broken but labour has not started
- Because there is a concern about your baby wellbeing
- Pregnancy concerns, for example:
- high blood pressure and/or protein in the urine (preeclampsia),
- diabetes (pre-existing or gestational GDM).
Induction of labour will affect your birth options and your experience of the birth process
- Your choice of place of birth will be limited, as you may be recommended interventions (like oxytocin infusion) that are not available for a home birth or in a Midwife-led Birth Centre
- You may be less likely to be able to use a birthing pool – that would depend on the pool availability on Delivery Suite and your personal risk factors.
- You may be slightly more likely to need an assisted vaginal birth (using forceps or ventouse), and slightly more likely to sustain severe perineal tear (OASI)
- An induced labour may increase the likelihood of requiring an epidural for pain management
- Your hospital stay may be longer than with a spontaneous labour
Before Induction
Membrane Sweep
In the days before an induction, you may be offered a membrane sweep to help you go into labour. This involves your midwife or doctor performing an internal examination and placing a finger into the cervix and making a circular, sweeping movement to separate the membranes that surround the baby, or massaging the cervix.
It may cause some discomfort, pain or light bleeding which is normal Stretch & Sweep is an intervention to bring on labour, however it is not recommended if your membranes have ruptured due to the increased risk of infection. You may be offered one membrane sweep every 48 hours, usually up to 3 sweeps can be performed in a week.
Research shows that having a membrane sweep can increase your chances of going into labour naturally by about 20%, without needing any further interventions.
Your doctor or midwife will ask for your consent before a membrane sweep. You do not have to agree. If you decide against it, they will respect your wishes and give you other options to get labour started.
What happens during induction?
Induction of labour occurs in stages or steps and it is a gradual process that might take from 2 to 5 days before your baby is born.
Step 1: Preparing your cervix (ripening)
Step 2: Breaking the waters (ARM)
Step 3: The Hormone drip
Where will my induction of labour happen?
Your doctor or midwife will talk to you about your options for where the step 1 can take place. This may be on the Delivery Suite, Day Assessment Unit or Antenatal Ward. The place of your induction will depend on yous and your baby risk factors.
On the day of your induction
Please come on the agreed date and time. Your birth partner can come with you at this time. Bring all your notes and scans with you as well as your labour bag. Please do not bring car seat at this time.
On arrival we will recheck that you and your baby are well and that nothing has changed since you were last seen. Your Midwife will discuss the care plan with you and explain the next steps.
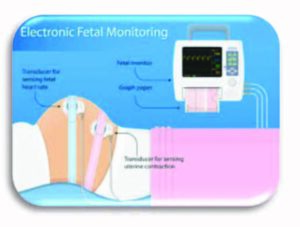
Monitoring your baby
Before we start the induction process, we recommend monitoring your baby’s heartbeat for around 30 minutes but sometimes it can be longer.
Two monitoring pads are positioned on your bump and held in place using wide elastic bands. The monitoring pads are attached to a cardiotogograph (CTG) machine, which records your baby’s heart rate and your contractions. Monitoring your baby heart is also recommended after the insertion of induction agent. Your midwife or doctor will discuss the process with you.
Vaginal examinations
The midwife or doctor will usually offer a vaginal examination at the start of the induction and then at a few points throughout the induction process to check how prepared for labour your cervix is. If your cervix is already ‘ready for labour’ (this is more likely if you have had vaginal births before), you may be ready to proceed directly to step two and have your waters broken.
If your cervix is not ready for the waters to be broken, there are a variety of methods that can be used to prepare the cervix. Your options will depend on your individual circumstances and preferences.
Step 1. Ripening the cervix
Dilapan S – Mechanical method for vaginal birth after caesarean (VBAC)
Dilapan are thin hydrogel rods that absorb fluid from the cervical tissue and expand within your cervix. A midwife or doctor uses a speculum (as in cervical smear tests,) to see the cervix and insert up to five rods. 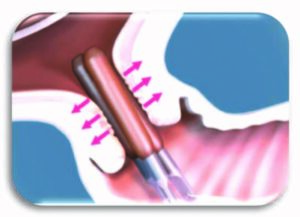
These can remain in for 12 to 24 hours. They are then removed during a vaginal examination. The rods contain no medicine or drugs, the focus is on expanding your cervix without them.
This method is especially recommended when you are planning vaginal birth after caesarean section.
Benefits and risks
- Least risk of hyperstimulation or scar rupture if planning VBAC
- The rods or tube could be uncomfortable to insert
- There’s a higher likelihood of needing an oxytocin drip and a longer time on drip
Propess pessary – hormonal method
A vaginal pessary which continually releases low doses of hormone to prepare the cervix. It looks like a small tampon and is inserted behind your cervix. The tape of the Propess can be felt at the opening of the vagina for easy removal and is intended to remain in place for 24 hours. After the Propess is inserted, labour may start straightaway, or it may take several days before your baby is born. Both reactions are normal as everyone reacts differently to the induction process.
If you have not gone into labour, or the cervix has not opened enough for your waters to be broken, after 24 hours you will be offered a Prostin gel.

Prostin gel
A low dose prostaglandin gel that is released into the vagina using a slim plastic applicator. It can be given every six hours, and is typically given up to 3 times, depending on how favourable (ready for labour) your cervix is.
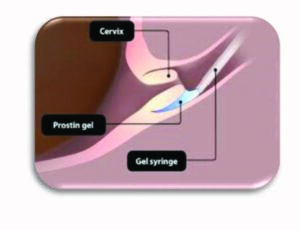
Risk of induction with prostaglandins
- Sometimes causes vaginal soreness.
- You might experience nausea, vomiting or diarrhoea.
- Very occasionally, hormone can cause the uterus (womb) to contract too much. If this happens, you will be given medication to relax the uterus.
- Most women will need further interventions (next step) to go into labour.
What happens next?
When you have completed step 1 and your midwife or doctor has found that your cervix is open enough to have your waters broken, we aim to transfer you to labour ward as soon as safely possible. Sometimes the waters break, or established labour
starts earlier during the induction process. This might mean that you are ready to go to the labour ward before the ‘end’ of step 1 of the induction.
Step 2: Breaking the waters (ARM)
This takes place on the Delivery Suite during a vaginal examination. The midwife will use a sterile instrument to rupture theamniotic sac (break your water). 
After this procedure, your midwife will monitor you and your baby’s heart rate. How long you will be monitored will depend on yours and your baby risk factors and the reasons for your induction.
After ARM you may be given some time, usually 2-4 hr to start contracting. If contractions don’t start after your water is broken, you’ll be offered a synthetic Oxytocin drip to start your contractions.
ARM success rate
For FIRST baby about 1 in 7 women will labour after an ARM without needing the hormone drip.
If you had vaginal birth before then about 1 in 3 or 4 will labour without needing the hormone drip.
If your induction does not work?
If your cervix does not open enough or you do not go into labour after first step your doctor will discuss the options with you. The options will be different depending on your and
your baby health.
Options might include caesarean section or sometimes we can stop induction, rest your body for 24 hr and then start the process again.
Step 3: The Hormone drip
Oxytocin is the hormone that causes contractions and cervical dilation during labour. Oxytocin is administer through small plastic tube into your vein (via drip). The midwife will monitor your contractions and adjust the oxytocin dosage accordingly.
Things to know:
- You may be restricted by the wires from the CTG if a wireless monitor is not available, but you can still stand, sit on a birthing ball, lay on your side or kneel on the bed with the monitor on.

- People have reported that the oxytocin drip is painful, so you may wish to consider your pain relief options before starting the drip.
- Sometimes oxytocin can cause the uterus to contract too frequently, we can reduce the rate at which it is being administered, stop the hormone drip and give you another drug to cancel the effect of the oxytocin if necessary.
How long does induction take?
The length of induction is different for every person and depends on how ready the neck of the womb is for birth. In general, it may take two to five days from the start of the induction for your baby to be born.
There may be delays in the induction of labour process as we need to ensure safety before proceeding at each step of the induction process.
Delays in transfer for ARM do happen and when they do, we will aim to keep you fully informed.
Additional resources and information
Recommendations | Inducing labour | Guidance | NICE
Visit the website or scan the QR code below:

Birthrights | Your human rights during pregnancy and childbirth
Visit the website or scan the QR code below:

Induction of Labour | AIMS
Visit the website or scan the QR code below:

Inducing Labour: Reasons, Methods and Side Effects
Visit the website or scan the QR code below:

Pain relief in labour, NCT
Visit the website or scan the QR code below:

Factsheet Managing labour: mood, mobilise and more
Visit the website or scan the QR code below:

Research
Induction of labour at or beyond 37 weeks’ gestation – Middleton, P – 2020 | Cochrane Library
Visit the website or scan the QR code below:

New evidence indicates early induction of labour may reduce inequalities in pregnancy outcomes | LSHTM
Visit the website or scan the QR code below:

Induction of labour at 41 weeks versus expectant management and induction of labour at 42 weeks (SWEPIS 2019) | The BMJ
Visit the website or scan the QR code below:

Research summary – an easy read version
Evidence on: Inducing for Due Dates – Evidence Based Birth®
Visit the website or scan the QR code below:

Birth Choice Clinic
To book a Birth Choice Clinic speak to your midwife.
Friend and Family Test (FFT) survey
Please fill in the Friend and Family Test survey to give your feedback about your maternity care including induction.
Bedford Hospital – complete the survey online or scan the QR code below:

Luton & Dunstable Hospital – complete the survey online or scan the QR code below:

Listening Service at Bedford Hospital
- Email: ListeningService@bedfordhospital.nhs.uk
- Call 01234 792095
Birth Reflection Clinic at L&D Hospital
- To book email: reflections@ldh.nhs.uk
Contact Patient Advice Liaison Service (PALS)
If you have a compliment, complaint or concern please contact Patient Advice Liaison Service (PALS).
Visit the PALS Bedford Hospital website page or scan the QR code:

Visit the L&D PALS website page or scan the QR code:

Important contact numbers
L&D
Maternity Triage Switchboard: 01582 329 574, Option 3. Maternity Triage
Bedford
Triage: 01234 795 805
