What is Keratoconus?
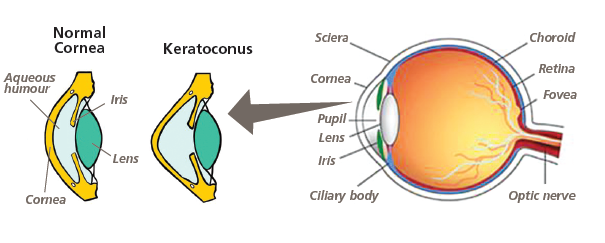
Keratoconus is an eye condition in which the clear covering of the eye (cornea) becomes thinner and weaker and begins to bulge, leading to blurred and distorted vision. Instead of having a curved football shape, it becomes pointed like a rugby ball.
It is a progressive condition- meaning that it continues to get worse. The rate of change is very variable. Generally, the later the onset of the condition, the more slowly it progresses and the earlier it stabilizes. Also, the rate of progression may vary between the two eyes.
What causes Keratoconus?
Both genetic and environmental factors are associated with Keratoconus. It may sometimes be inherited in an autosomal recessive pattern. It is known to be associated with conditions like eczema, hay fever and asthma. Eye rubbing is known to worsen the condition and should be avoided.
When is it diagnosed?
Depending on the ethnicity, it affects 1 in 2000 to 1 in 450 people and is more common in non-Caucasians. It is usually diagnosed in young people at puberty, in their late teens or early twenties.
How is it diagnosed?
Usually, the following tests are done to diagnose this condition:
- Eye refraction at the opticians.
- Slit lamp examination.
- Keratometry
- Computerised corneal mapping (pentacam)
How is it treated?
There is no cure for Keratoconus. It cannot be treated with any eye drops or medicine.
The various treatment options are:
- Glasses: In the early stages, these help to improve the vision.
- Contact lenses: If the vision does not improve with glasses, different type of contact lenses can be tried (rigid lenses or special lenses).
- Collagen Cross Linking: For progressive Keratoconus, this helps to strengthen a weak cornea and reduce any further deterioration. This does not improve the vision.
- Intracorneal rings: When there is intolerance to contact lenses or when the condition continues to progress, these rings may be inserted to reinforce the cornea and reshape it.
- Corneal Transplant: In advanced cases, either a partial thickness graft (Deep Anterior Lamellar keratoplasty) or full thickness graft (Penetrating Keratoplasty) may be necessary.
Can it cause blindness?
Keratoconus does not cause complete blindness. It is difficult to predict how rapidly the condition will progress in any individual, but most patients don’t require surgery.
Sometimes, the cornea can become so thin that a break within causes fluid to build up, causing clouding of vision and can be painful. This needs prompt attention from a doctor and can cause scarring.
If you would like any further information, please discuss it with a doctor in our clinic.
