- Ongoing high blood glucose can seriously damage your eyes, heart, kidneys and nerves.
- Keep your blood glucose between 4 and 7 as much as you can to protect your long term health.
- HbA1c tells us if your blood glucose is high enough to be damaging.
- Aim for an HbA1c of less than 58mmol/mol (7.5%) to protect your long-term health.
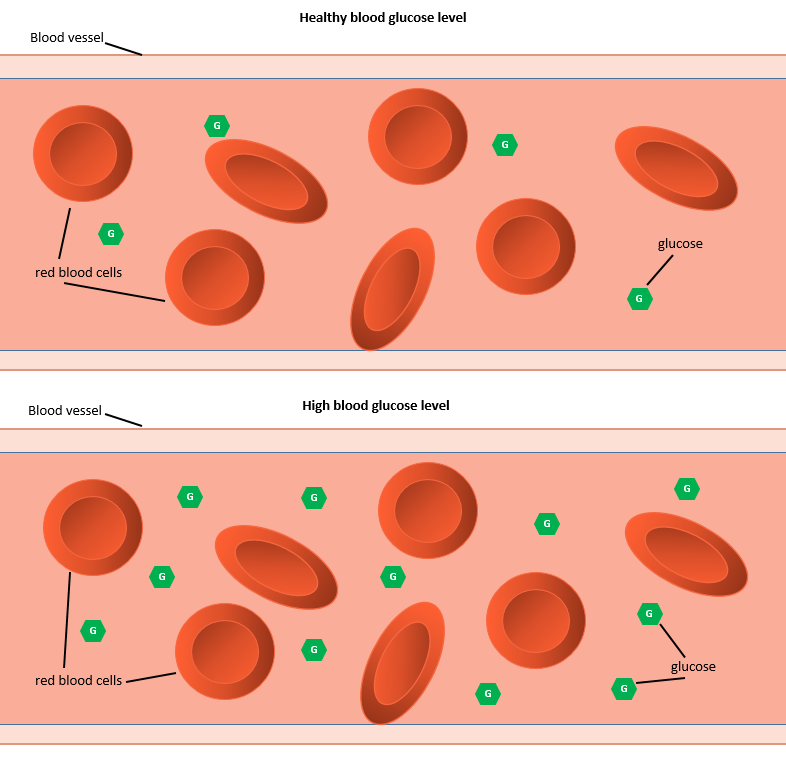
Type 1 diabetes affects your long-term health when you take too little insulin or take it at the wrong time.
Your body needs insulin to move glucose out of your blood and into your muscles.
If your body doesn’t get insulin when it needs it, the glucose builds up in your blood.
The glucose sticks to the haemoglobin in your blood, making it chunky and jagged. When this happens, it starts to damage blood vessels all over your body.
This can cause problems in your eyes, heart, kidneys, gums, feet, nerves and private parts.
Some of these problems can make you very ill. They are called complications of diabetes.
How will I know if I am getting complications of diabetes?
The damage to blood vessels happens whenever your blood glucose stays high for prolonged periods of time, even if you are young, but the damage to your body parts will usually only be noticeable after you turn 12.
So, when you turn 12, we will offer you three checks for these complications of diabetes:
- A urine test: We will ask you to pee into a bottle (ideally first thing in the morning) to check your kidneys are healthy
- A foot check: we will look at and gently feel your feet to check your blood circulation.
- Your GP will refer you for diabetic eye screening. The eye doctors will test for “retinopathy”, to check your eyes are heathy.
We want to spot any problems as soon as possible so that we can give you medicine to make it better and work with you to keep your blood glucose in your target range.
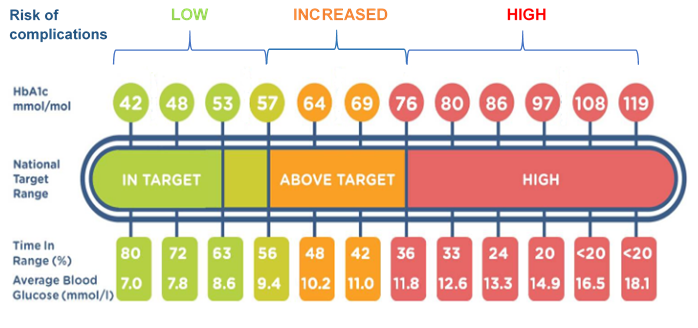
HbA1c and Time in Range
HbA1c is a count of how much glucose is stuck to the haemoglobin in your blood.
This is what damages your blood vessels when your blood glucose stays high for a long time.
If your HbA1c is below 58mmol/mol, you have the same level of risk as someone without diabetes.
If your Hba1c is above 60mmol/mol and especially if your HbA1c goes above 75mmol/mol it means that the extra glucose in your blood will start to damage your blood vessels.
We will help you make changes to your diabetes routine to lower your HbA1c and keep it as low as possible for your future comfort and good health.
HbA1c can only be measured in the hospital and it changes slowly so we only measure it every 3 months.
You can check your Time in Range at home and it’s calculated weekly.
Time in Range is a great way to keep track of your blood glucose levels between clinics and make changes as needed.
The picture below shows how HbA1c, Time in Range, average blood glucose and the risk of complications are all linked:
What can I do to prevent complications of diabetes?
- Check your blood glucose at least 5 times a day
- Use diabetes technology to make your routine quicker, easier and more accurate
- Work out your meal time carbs carefully so that you get just the right amount of insulin
- Contact the diabetes team regularly to make sure your treatment routine is right for you
- Come to all your appointments. Come on time and do all of the tests that are offered. This is so that we can give you time and attention to get your diabetes routine just right for you.
- Your diabetes nurse will talk to you about diabetes care at nursery / school
- Call your diabetes nurse if you have any questions or concerns about diabetes care away from home.
School / nursery
 You can join in all normal school activities, including school trips.
You can join in all normal school activities, including school trips.
Your diabetes nurse will create an individual health care plan for you. This resource explains how your school/ nursery team will help you manage your diabetes.
We will work together to update your care plan each September, and whenever your treatment changes.
Our nurses will visit the school to train the teachers and support staff so they can help you when you start school.
If you need help with your injections the nurse will train the school/nursery staff individually to make sure they can do the injections safely and well.
If you have insulin injections at school, you will need to leave a spare insulin pen and injecting equipment at school.
On holiday / travelling
 Always consider your diabetes when planning your holidays.
Always consider your diabetes when planning your holidays.
If you are staying in the UK, and not flying, you may not need to make any changes to your insulin.
If you are going on an activity holiday, you may need to adjust your insulin doses to compensate for this. Please ask us for advice at clinic, or phone for advice.
If you are travelling abroad, always take:
- Extra insulin and needles (in case you lose or damage your pens)
- Extra testing equipment (to monitor your diabetes whilst away)
- Consider ID if you are going away with the school or friends.
- Snacks and hypo treatment for the journey (in case there is a delay or you don’t like the food)
If you are flying
- Always take your insulin in your hand luggage. Do not put it in your main case as it will freeze.
- Ask your diabetes nurse for a letter which will explain why you are carrying needles and liquids on the flight
If you visit a hot country
- You may need to take less insulin. Call your diabetes nurse two weeks before you travel to plan this.
- Keep your insulin in a fridge. But when you get home only use the insulin for two weeks and then throw it away. This is because it has not been refrigerated on the journey and so will expire after one month.
- If you will not have a fridge whilst on holiday, FRIO bags are useful. These can be purchased on line or at a chemist to keep insulin cool whilst abroad.
Time Zones
For travelling to Europe, you will be able to take your basal insulin at similar times.
If you are travelling to the USA, or ASIA, Because your sleep and waking times will be changing to the local time, you will need to change the times and doses of your basal insulin. Call your diabetes nurse two weeks before you travel to plan this. Have your flight times and durations available as your diabetes nurse will need these to work out your timings.
Travel Insurance
Declare your diabetes on the travel insurance, to make sure you are covered if you become ill while you are away. Some companies may charge extra for this. You can get a quote through Diabetes UK travel insurance, which may be cheaper than your usual supplier. (insuremydiabetes.org.uk or call 08081688711)
- Let your diabetes team know how you are feeling, we can help
- Learn more about diabetes to understand what is happening
- Make time to enjoy yourself: it’s good for you
- Ask your diabetes nurse about psychology support
Talk about it
Talk to your friends, family and your diabetes team about how you feel. If that seems scary, write down or draw how you feel.
Let us know how you are feeling. We are all here to help you. We can help you by talking things through, finding solutions to practical problems, or referring you for group work or 1:1 psychology sessions.
If you are 11 or older, you can join Together Type 1 which is a great place to meet others, share problems and get support.
Parents can join the Diabetes UK support forum to get advice and support from other parents
There is useful information for parents on Diabetes UK.
You can also call or email the Diabetes UK helpline for confidential advice and support
- Call: 0345 123 2399, Monday to Friday, 9am to 6pm
- Email: helpline@diabetes.org.uk
Ask lots of questions
It can take a while to get used to having diabetes. We are here to help you every step of the way. If you have any questions just ask, even if they seem silly or pointless! You can call or text your diabetes nurse.
Even if you have had diabetes for a while, the way you manage it will change as you grow and change the diabetes team are always ready to answer your questions.
Have fun
Make time to have fun together as a family, or with friends.
It can be chilled or active, simple or grand. If you need help working out your diabetes management for this, just call your diabetes nurse. We can help you plan for eating out, going to parties, having sleepovers, camping out, or doing something physically active.
Whatever you want to do, we can help you plan for it so you can focus on the fun.
Maybe you can’t do everything exactly the same way you did before diabetes, but we are all here to help you find new ways of doing your favourite things.


Ask your diabetes team about psychology support
Megan and her team of children’s psychologists are here to help you with your diabetes related concerns. The team run support groups and sessions throughout the year. They can refer you to other health and wellbeing services in the area, and they can support you in one to one sessions if you need it. Ask your diabetes team about what psychology support is available to start the process.
- Keep a simple regular routine
- Do some regular exercise that you enjoy
- Get plenty of rest
- Keep doing things you enjoy and explore new things
- Eat a balanced diet. Call or email Michaela if you would like a dietetic review
Keep a simple regular routine
Eating and taking your insulin at regular times each day makes it easier to follow your routine.
Use lists and labels to make everything as easy as possible for yourself.
When you are away from home, try to stick to the same routine, if possible, to make your life easier.
Do some exercise that you enjoy
Exercise helps blood glucose stay more stable over time. It makes you feel good and it helps keep your heart and blood vessels healthy.
Make sure you prepare for exercise by checking your blood glucose before you start and having a SMALL snack if needed.
Get plenty of rest
At night, your body repairs itself and cleans out toxins. You can help your body by making sure you go to bed on time.
Managing your diabetes at night can often lead to missed sleep, and when you are tired, it’s easy to let your diabetes routine slip.
If you notice this happening, go to bed a little earlier, and make time in the day to prioritise your diabetes routine and to rest and relax.
Keep doing all the things you enjoy and explore new things
If you feel like diabetes is stopping you from doing the things you enjoy, speak to your diabetes nurse. We want you to be happy and healthy with diabetes, and we are here to help you.
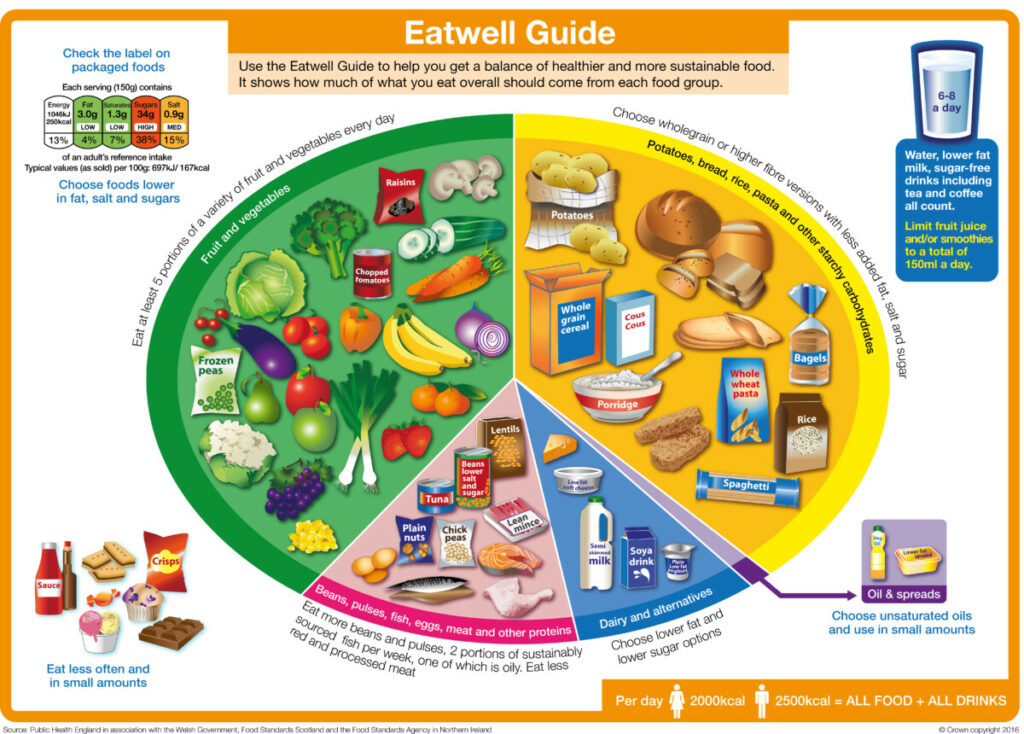
Eat a good balance of foods and enjoy your meal times
You don’t need to eat anything different because you have diabetes. The NHS advice on what to eat is the same as for all young people.
You can read more on the NHS website.
We have included the Eatwell poster for you below which shows the different food groups and how to balance your meals.
Contact Michaela, our children’s diabetes dietitian, for personalised help and advice. Michaela will help you learn to carb count so you can work out how many carbohydrates are in your food and get your insulin doses just right for your individual needs.
You can contact Michaela on 07974596060 or email michaela.goodwin@ldh.nhs.uk
Digibete have carb counted some delicious European and South Indian recipes to make life a little easier for you.
Diabetes Systems and Apps
- Glooko pro connect code: enldhpaed
- LibreView code: 01166469
- DigiBete code: MZRVD
Needle Disposal
You will need a sharps box, to dispose of needles and lancets. Call your local council to get one delivered.
- LUTON:
- 01582 546812
- wastecustomerservice@luton.gov.uk
- DUNSTABLE/LEIGHTON BUZZARD:
- 0300 3008000
- customers@centralbedfordshire.gov.uk
- HERTFORDSHIRE:
- 0300 1234051
- csc.wasteaware@hertfordshire.gov.uk
Financial Help
You can claim for Disability Living Allowance (DLA). Let your diabetes nurse know if you need help to fill this in. Get the form from the website https://www.gov.uk/disability-living-allowance-children/print or call 0800 121 4600
Prescription Items
You will get your diabetes care supplies on a repeat prescription. It usually takes 2 days for the GP to provide a prescription. Make sure to request a repeat prescription at least 2 days before you need it.
Tell your GP as soon as your prescription changes, so they can change the items on your list.
Vaccines
As well as the usual childhood vaccines, we recommend that your child has the flu jab each autumn. You can still have any vaccinations required for travel purposes, they should not affect the diabetes. Speak to your diabetes nurse if you have any questions about this.
Small Snacks (10g Carbohydrate)
You can eat snacks which have less than 10g of carbohydrate between meals without insulin or if your blood glucose is getting low.
If you feel very hungry, have a small snack and, over time, increase the amount of food you eat at meals so you don’t need to snack. Have plenty to drink between meals and try to keep snacks to a minimum. you can call Michaela, your children’s diabetes dietitian for help with meal ideas to keep you feeling fuller for longer.
The list below shows some lower-carbohydrate and carbohydrate-free snacks to have if you feel hungry between meals or need a small snack to raise your blood glucose.
If you eat more than 10 grams of carbohydrate you will need to take bolus insulin
Salad/vegetables
Veg slices, e.g. pepper, celery, carrot
- Quantity: Small plate
- Carbs (g): 0
Salad, e.g. cucumber, lettuce, spring onion, radishes, olives, avocado, cherry tomatoes
- Quantity:
- Carbs (g): 0
Meat/fish
Plain chicken drumsticks (no breadcrumbs)
- Quantity: 1-2
- Carbs (g): 0
Tinned cream of chicken soup
- Quantity: 1/2 tin
- Carbs (g): 5
Tinned fish
- Quantity: 1/2 tin
- Carbs (g): 0
Fish fingers
- Quantity: 2
- Carbs (g): 6
Vegetarian alternatives
Mini vegetable samosa
- Quantity: 1
- Carbs (g): 6
Quorn sausage (plain, not Cumberland)
- Quantity: 2
- Carbs (g): 8
Quorn cocktail sausages
- Quantity: 4
- Carbs (g): 7
Marinated tofu
- Quantity: 100g
- Carbs (g): 0
Tomato/vegetable soup
- Quantity: 1/2 tin
- Carbs (g): 10
Eggs
Scrambled egg/boiled/poached egg
- Quantity: 1-2
- Carbs (g): 0
Plain/cheese/ham/veg (not potato) omelette
- Quantity: 2 eggs
- Carbs (g): 0
Cheese
Cheese string (20g)
- Quantity: 1
- Carbs (g): 0
Mini Babybel
- Quantity: 1
- Carbs (g): 0
Soft Cheese Triangle
- Quantity: 1
- Carbs (g): 0
Cheddar cheese, edam, Red Leicester, Mozzarella, cream cheese
- Quantity: 25g/matchbox-sized piece
- Carbs (g): 0
Crisps/nuts/popcorn
Mixed unsalted nuts – Whole peanuts or whole nuts should never be given to children under five because of the risk of choking
- Quantity: 50g/handful
- Carbs (g): 0
Wotsits (17g multipack packet)
- Quantity: 1 packet
- Carbs (g): 9
Skips (13g multipack packet)
- Quantity: 1 packet
- Carbs (g): 8
Plain popcorn
- Quantity: 20g
- Carbs (g): 10
“Skinny” popcorn Sweet ‘n’ salt (17g multipack packet)
- Quantity: 1 packet
- Carbs (g): 9
Butterkist Sweet Cinema Style (12g multipack packet)
- Quantity: 1 packet
- Carbs (g): 8
Pombears
- Quantity: 1 packet (13g)
- Carbs (g): 8.2
Breads/crackers
Plain rice cake (not thick)
- Quantity: 2
- Carbs (g): 10
Oat cake
- Quantity: 2
- Carbs (g): 10
Cheddar biscuits (5g)
- Quantity: 2
- Carbs (g): 6
Bread sticks (5g)
- Quantity: 2
- Carbs (g): 8
Cream crackers (8g)
- Quantity: 2
- Carbs (g): 10
Water biscuits (6g)
- Quantity:
- Carbs (g):
Puffed wheat crackers (9g)
- Quantity: 2
- Carbs (g): 10
Thinly sliced bread (22g)
- Quantity: 1
- Carbs (g): 10
Crisp bread (10g)
- Quantity: 1
- Carbs (g): 7
Cracker bread
- Quantity: 2
- Carbs (g): 8
Dips and Spreads
Houmous
- Quantity: 2 tbsp
- Carbs (g): 0
Guacamole
- Quantity: 2 tbsp
- Carbs (g): 0
Salsa
- Quantity: 2 tbsp
- Carbs (g): 0
Nut butters e.g. peanut, cashew, almond (choose sugar-free)
- Quantity: 1 tbsp
- Carbs (g):0
Marmite
- Quantity: 2 teaspoons
- Carbs (g): 2
Yoghurts
Natural yoghurt (100g)
- Quantity: 1
- Carbs (g): 7
Plain Greek yoghurt (100g)
- Quantity: 1
- Carbs (g): 6
Diet/Light yoghurts such as Weight Watchers (125ml)
- Quantity: 1
- Carbs (g): <10
Fromage-frais (45g pot)
- Quantity: 1
- Carbs (g): 6
Children’s yoghurts such as Frube or Choobs (40g)
- Quantity: 1
- Carbs (g): 6
Children’s yoghurt pouches (70g)
- Quantity: 1
- Carbs (g): 9
Fruits
‘Fun size’ small apple (85g)
- Quantity: 1
- Carbs (g): 10
Average sized apple (131g)
- Quantity: 1/2
- Carbs (g): 10
Clementine’s (80g)
- Quantity: 2
- Carbs (g): 10
Satsuma (160g)
- Quantity: 1
- Carbs (g): 10
Grapes
- Quantity: 10
- Carbs (g): 10
Fresh Apricots
- Quantity: 2
- Carbs (g): 8
Kiwi
- Quantity: 2
- Carbs (g): 10
Orange
- Quantity:1
- Carbs (g): 7
Peach
- Quantity: 1
- Carbs (g): 10
Small pear (100g)
- Quantity: 1
- Carbs (g): 10
Strawberries
- Quantity: 7
- Carbs (g): 5
Blueberries
- Quantity: 15
- Carbs (g): 5
Raspberries
- Quantity: 15
- Carbs (g): 3
Small plum
- Quantity: 2
- Carbs (g): 10
Raisins (15g)
- Quantity: 1 small box
- Carbs (g): 10
Biscuits
Malted milk biscuits
- Quantity: 2
- Carbs (g): 10
Rich tea biscuits
- Quantity: 2
- Carbs (g): 10
Nice biscuit
- Quantity: 2
- Carbs (g): 10
Jelly/Ice lollies
Sugar-free ice lollies (can be homemade)
- Quantity: 1
- Carbs (g): <4
Sugar-free jelly
- Quantity: 1
- Carbs (g): <2
Diabetes UK
We provide information, advice and support to help people with diabetes manage the condition well, and bring people together for support when it’s needed most.
Other languages
Available languages are: Arabic, Bengali, Braille, British Sign Language (BSL), Easy Read, English, French, Gujurati, Hindi, Large print, Polish, Punjabi, Romanian, Simplified Chinese, Somali, Tamil, traditional Chinese, Urdu, Welsh
Together Type 1
Youth programme for 11-25 year olds: “we are there to support each other no matter what. Join us to meet new friends, learn new skills, and build your confidence.”
Digibete website and App
A place to help young people, families and communities to manage Type 1 Diabetes.
Essentials videos in different languages
For other languages visit https://www.digibete.org/essentials/ and scroll down for British Sign Language, Arabic, Bengali, Chinese, Polish, Somali, Tamil, Urdu, Spanish, French, Ukrainian, Punjabi.
Digibete App
This is free. It has all the benefits of the website along with a place to store all your important diabetes information and messages and updates from your Diabetes team.
You can download the App from App store or Google Play. Sign up using your clinic code: MZRVD. Sign up with an email address and a password that can be shared with carers. Up to 6 devices can the access the same App.
JDRF
JDRF, As the leading global type 1 diabetes charity, aim to help people live better with the condition, prevent people ever developing it and one day, find cures. They do this by funding research, campaigning for access to all treatments and connecting and supporting the type 1 community.
