Physiotherapy – Looking after your Pelvic Health in Pregnancy
Looking after your Pelvic Health in Pregnancy
This leaflet will explain the importance of ensuring good pelvic health including what the pelvic floor muscles do and how to exercise them, what symptoms to look out for and how to access help and support if things ‘aren’t right’.
Getting things right before problems start has been shown to improve our pelvic health as we get older – reducing the risk of urinary (wee) and faecal (poo) leakage, as well as helping to prevent prolapse developing.
It is quite common to experience incontinence during pregnancy and after having a baby, but it is not ‘normal’.
- 40-50% of women in their 2nd and 3rd trimesters of pregnancy and immediately after birth have urinary leakage
- 1 in 10 of pregnant women can also have anal incontinence (leakage of poo or wind)
- 1 in 12 of women have problems with pelvic organ prolapse
- If not treated 1 in 5 women still have symptoms at 12 months post-natal
These symptoms can be prevented by doing pelvic floor muscle exercises during pregnancy – starting as early as 16 weeks of pregnancy. Should you still have incontinence issues following delivery, by continuing the exercises after having your baby, the issues can also be resolved.
Where are the pelvic floor muscles?
The pelvic floor is a group of muscles like a hammock at the base of the pelvis, running from the pubic bone at the front to the tailbone at the back.
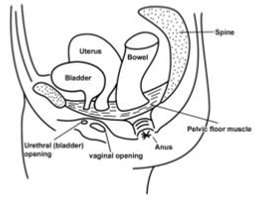
Illustrated diagram of pelvic floor
It has three openings:
- The urethra (the bladder outlet)
- The vagina (birth canal)
- The anus (back passage)
What do they do?
- These muscles support the pelvic organs (bladder, uterus (womb) and bowels) to reduce the risk of prolapse. They also help to control the bladder and bowels.
- Healthy pelvic floor muscles may also help improve your sex life.
- Pelvic floor muscles should be kept strong just like any other muscle within the body.
What can weaken the pelvic floor?
- Pregnancy
- Childbirth (especially with assisted vaginal births, episiotomies, perineal tears or a very large baby)
- Straining regularly to open your bowels (constipation)
- Repeated heavy lifting
- Changes during the menopause
- Chronic cough, e.g. associated with smoking or respiratory conditions
- General lack of fitness
- Being overweight
- Long periods of inactivity (due to illness / surgery)
- High impact, vigorous exercise or with heavy weights
Symptoms to look out for:
- Leaking urine (wee) on coughing, sneezing, lifting or running (even small amounts)
- Sudden urgent or frequent need to pass urine (wee)
- Feeling ‘something coming down’ or a ‘dragging sensation’ in the vagina – (prolapse)
- Being unable to control leakage of wind or ‘poo’ from the bowel
- Lack of sensation with sex
- Pain with sex
How do I find my pelvic floor muscles?
It is important to know you are exercising the right pelvic floor muscles.
Find a comfortable position sitting upright with your feet flat on the floor.
Imagine that you are trying to stop yourself passing wind and urine at the same time, drawing the muscles upwards and forwards starting from the back passage.
It is important not to hold your breath.
How to exercise the muscles?
Hold this squeeze for 5–10 seconds and then relax fully for 5 seconds. This is called a slow squeeze.
Repeat this 5 –10 times until you feel the muscles tiring.
Now squeeze your muscles in the same way but relax after 1-2 seconds, let go and repeat 5-10 times. This is called a quick squeeze.
You should aim to do 5 –10 slow and quick squeezes at least 2 times per day.
You should continue these exercises throughout your pregnancy and after you have had your baby.
This will help to prevent future problems such as bladder leaking and prolapse.
When to get help?
Should you continue to have symptoms of bladder (wee) leaking, prolapse, bowel urgency or leakage (wind or poo) or pain with sex during pregnancy or after having your baby you can ask your midwife, health visitor or GP to refer you to the pelvic health physiotherapy team.
General advice for healthy bladder, bowel and pelvic floor muscles
- If you are doing these exercises after delivery and you have a catheter (a tube to empty your bladder) make sure you wait for the catheter to be removed before starting pelvic floor exercises
- Pelvic floor exercises can be started gently on the first day after you have your baby – whether the birth was vaginal or by c-section – unless you are told otherwise
- Try to tighten your pelvic floor muscles prior to any activity that requires effort (e.g coughing, sneezing, lifting – washing/hoovers or your baby!) to prevent leakage of urine and vaginal prolapse
- Ensure each pelvic floor contraction is fully relaxed before doing the next
- Avoid caffeinated drinks (e.g. tea, green, tea, coke, energy drinks) and fizzy drinks as they can irritate the bladder
- Try to drink 1.5-2 litres of fluids a day but remember if it is very hot or you are breastfeeding you must increase the amount of fluid you drink
- Download the NHS Squeezy App available on all smartphones and mobile devices to help you to do the exercises – remember to reduce the pre-set programme to the programme overleaf
- Avoid constipation by drinking adequate fluids, taking regular exercise (just walking helps) and eating a good, varied diet containing fruit, vegetables and wholegrains (e.g brown rice / porridge). Speak to your GP if it is a long-standing problem
Other symptoms during pregnancy or post-natally
Pelvic girdle pain or low back pain in pregnancy
About 1 in 5 pregnant women are affected by pelvic girdle pain to some degree.
It is important to remember that it may not get worse through pregnancy and treatment early in pregnancy can help to manage symptoms well.
It does not mean you cannot have a normal labour or delivery.
Pain may be felt around your hips, the front or back of your pelvis or down into your buttocks.
Perineal massage
About 85% of women who have a vaginal birth will have some degree of perineal injury or tear that may require stitches. Mostly these heal well with no problems, however some may lead to further issue without the correct support. Perineal massage done from 35 weeks of pregnancy has been shown to help reduce the level of injury or tear experienced. For more information speak to your Midwife or refer to our www.bedfordshirehospitals.nhs.uk/our-services/maternity-2/pelvic-health/
Diastasis Recti
During pregnancy, the abdominal (tummy) muscles are stretched with baby’s growth and the linea alba (the tissue in the middle of your tummy) gets softer, this causes diastasis recti. During pregnancy you may see your tummy ‘doming’ when you sit up in bed or get out of the bath – if this happens, try to roll onto your side to get up as this may help it getting worse and is likely to reduce any back soreness associated with it.
Normally a small diastasis will recover on its own by 8 weeks postnatal. Sometimes a large diastasis may take up to 12months to resolve and require some guidance from a specialist physiotherapist.
Your midwife or GP can refer you to pelvic health physiotherapy for further support with this.
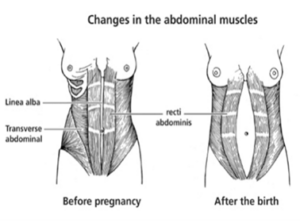
Illustrated diagram of changes in the abdominal muscles
Further information on all these pregnancy and post-natal issues can be found at www.thepogp.co.uk
Please scan the below QR codes for the direct web links for all resources mentioned in this booklet or use the following links:
- Pelvic Health Page | Bedfordshire Hospitals
- Pelvic health videos for pregnancy and the postnatal period | Bedfordshire Hospitals
- POGP Website
- The Squeezy App
