This information leaflet is for patients who are having a therapeutic examination of the bowel (known as a Therapeutic Colonoscopy). This leaflet explains the reasons for the examination, what is involved, and about any possible risks or side effects.
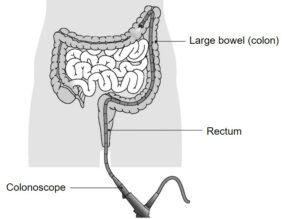
A colonoscopy is an examination of the inside of the large bowel using a long flexible instrument called a colonoscope. This is introduced into the colon via the back passage and an image is projected via a small camera onto a screen.
Reasons for having this examination include
- To resect (remove) polyps
- To re-examine any previous problems
What is a polyp?
A polyp is a protrusion (abnormal growths of tissue) from the lining of the bowel. If a polyp is found, or if we already know you have a polyp, it is usually removed by the Endoscopist as some polyps can also cause problems in the future. Following your previous procedure, a large polyp has been detected and therefore requires resection.
There are 2 techniques which might be used to remove large polyps (abnormal growths of tissue) from the lining of the intestinal wall. They are Endoscopic Mucosal Resection (EMR) and Endoscopic Submucosal Dissection (ESD). Both procedures can be undertaken during a gastroscopy, flexible sigmoidoscopy or colonoscopy procedure. It is important for you to be comfortable during the procedure and to remain still; therefore your consultant will discuss whether a light sedative (conscious sedation) or deep sedation is required.
It is imperative that you read and follow the instructions contained within this information leaflet, relating to the particular procedure you are undergoing. If you have any further questions, a member of the Endoscopy team will be more than happy to discuss these with you.
What is EMR?
EMR is the most commonly used technique for removal of large polyps. It involves injecting a fluid solution under the polyp to lift it away from the underlying muscle (forming a protective cushion); a snare is then placed over the polyp to remove it. As there are no nerve endings within the lining of the bowel wall you will not feel any pain. However, despite this being a relatively quick procedure, it is not always possible to remove the polyp in one piece, which may cause the polyp to recur at a later date.
What is ESD?
ESD is a more advanced endoscopic technique for removal of large polyps. One of the main advantages of this procedure, over other types of polyp removal procedures (notably EMR), is that the polyp is removed in a single piece. This provides assurance whether the polyp has been completely removed of all the abnormal cells and therefore can be used to better predict when future endoscopic (surveillance) procedures may be required.
What does ESD involve?
The ESD procedure will be done by a specially trained Endoscopist and is similar to EMR as it involves injection a fluid solution under the polyp to lift it away from the underlying muscle (forming a protective cushion). After this has been performed, special equipment is used to remove the polyp all in one piece. The polyp is then retrieved and sent to the laboratory for analysis. You may experience some bloating or discomfort during or after the procedure which will be manage with a strong painkiller and sedatives. You will be monitored carefully during and after the procedure. The procedure does take longer than other polyp removal techniques; between one and four hours to complete. In most cases you should be able to go home on the same day, but on occasions a short stay in hospital may be required.
Preparation for the examination
For this examination to be successful your bowel must be as empty as possible. You will be given a potent laxative (instructions for this will be provided separately) and a recommended change in diet for a few days before the test. It is very important to follow these instructions carefully and drink plenty of fluids on the day before the examination.
Patients must not stop any prescribed medication including blood pressure tablets unless advised by your consultant. If you are however on any iron preparations or medication that may make you constipated, this must be stopped 7-10 days before your procedure.
If you have diabetes, or you are taking anticoagulants (blood thinning medication) such as Warfarin, Ticagrelor Clopidogrel, Dabigatran, Rivaroxaban, Edoxaban or Apixaban, you will be given specific instructions in advance. Patients who continue to take Warfarin, or who have stopped Warfarin just before the test, will need to have a blood test on the day in the unit.
Please read and complete your medical assessment form in advance of your procedure. You will also be sent a consent form which a nurse will discuss with you on the day.
If you have not been advised what to do about your medicines or if you require any additional access or support, please call 07815 178199
Mon-Sun between 10:30-11:30am and 14:30-15:30pm only. Outside of these hours, this telephone is for Emergency calls only.
On arrival at the hospital
- Please go straight to the Endoscopy Unit and ring the bell to let the staff know you have arrived
- Procedure times can be unpredictable so you may have
- to wait a while, it is a good idea to bring something to read
- A nurse will discuss your medical history with you, while also checking your pulse, blood pressure, oxygen levels, blood sugar (if diabetic) and clotting (if on anticoagulants). They will ask any necessary additional questions and you will have the chance to ask anything you may want to know
- The nurse will discuss the consent form with you, to confirm that you understand the procedure and agree to go ahead with it, after which you should sign the form. You will be given an identity band which you should also check for accuracy
- You will then be asked to undress into a hospital gown. Put on
- your dressing gown over this and wait until you are taken through to the examination room
- A nurse will remain with you throughout the examination.
The examination
Most procedures require sedation and/or a painkiller which is given as an injection to make you as relaxed and comfortable as possible. Sedation may also make you feel sleepy but for most patients it induces sleep after the examination, rather than during it.
We will monitor your heart rate and breathing throughout. If you are having a deep sedation, there are some additional risks to be aware of. These will be discussed when you are reviewed by the anaesthetist.
In order to have sedation and/or pain relief it is important that you have a responsible adult to look after you for 24 hours after your colonoscopy. Throughout the test you also may be given oxygen via a nasal tube.
While you are lying comfortably on your left side on the examination trolley, the doctor or nurse specialist will gently pass the small flexible tube (colonoscope) into your large bowel via the back passage.
Some air is passed into the bowel to expand it to allow for a clear view. This can cause some discomfort but it will not last long. You may feel as if you want to go to the toilet but be reassured that this will not happen. Most of the air will be sucked out at the end of the test.
The bowel can be very long and bendy, so manoeuvring the tube around it can take time and may cause some discomfort and stretching. In order to complete the examination it is occasionally necessary to change your position onto your front, back or right side. An assistant may have to press on your abdomen to assist the procedure.
Air that has been passed up into the bowel will have to come out again as wind. Please do not worry about this, it is quite normal.
After the examination
You will be taken to the recovery area. Once recovered from the effect of the sedation and the procedure, you will be offered a drink and a biscuit.
A nurse will explain the findings of your procedure and you will be given a copy of your report before being discharged. It would be a good idea for an adult member of your family or a friend to be present as you may not remember everything you have been told.
You may experience some more discomfort from wind – this should settle after a few hours.
The sedative effects (if administered), may make you sleepy and can last for 24 hours. Even though you may feel alert you must be accompanied home. If you had the sedative injection and/or analgesia, you must have a responsible friend or relative to take you home and stay with you for 24 hours. If this is a problem, please telephone the department as soon as possible. For 24 hours post procedure you must not drive a car, drink any alcohol, sign any legally binding documents, operate machinery and/or look after any dependents.
Individuals are unable to donate blood for 4-6 months following any endoscopic procedure. (British Society of Gastroenterology Guidance; updated February 2020)
The risks
Colonoscopy is a safe procedure but there can be a risk of the following:
- Bowel preparation can cause immediate problems with the kidneys, particularly in patients with known kidney problems or those who are on medication that affects the kidneys. This can usually be treated, however very rarely there may be permanent damage. Women taking the oral contraceptive pill should be aware that taking bowel preparation might prevent the absorption of the pill. Additional contraceptive precautions should be taken until the next period begins.
- Occasionally it is not possible to remove the polyp or to remove it in one piece (the latter is uncommon and the alternatives will be discussed with you after the procedure).
- Occasionally patients may develop pain in the abdomen related to electro- cautery and/or trapped wind.
- More serious complications include a tear or hole in the bowel wall (called a perforation) or bleeding.
- EMR: 1 in 20 risk of bleeding, 1 in 200 risk of perforation (small tears may be repaired during the procedure, larger tears might require an operation to repair it) and 5% chance of polyp recurrence.
- ESD: 1 in 20 risk of bleeding or perforation (small tears that can be repaired during the procedure, however, 1 in 75 cases there may be a major tear that requires an operation to repair it).
- There is a 1 in 20 chance of hospital admission for observation post- procedure for if there are any concerns related to delayed bleeding or perforation.
- It is important to note that these problems can occur up to two weeks after the procedure (see advice below) and you should therefore not take any long haul travel for this time period.
- Sedation lowers blood pressure and can cause short term problems with breathing and heart rate. Before discharge you will be monitored carefully so that if any problems do occur they can be treated quickly. Older people and those with pre-existing conditions may be at higher risk
If you have any concerns about these risks please talk to your specialist before your colonoscopy.
Alternative procedures
The alternative options to this procedure are:
- Surgical removal of the polyp
- Not treating the polyp
If you have any concerns about EMR or ESD, please discuss them with your consultant.
Air travel
If you have undergone a therapeutic procedure, you should not undertake any air travel for 2 weeks after your procedure. You will be advised on discharge which procedure you have had.
Sleep Apnoea
Please bring your CPAP machine with you for your appointment because if you choose to have sedative injection, due to the possible side effects, it might be necessary for it to be used to ensure your safety.
Pacemaker Device or Implantable Cardioverter Defibrillator (ICD)
Please bring your pacemaker device or implantable cardioverter defibrillator manufacture information card with you a cardiac technician might be required and will need that information to make sure your device is safe for you during this procedure.
Having a procedure with a training Endoscopist
Endoscopy Training at Luton and Dunstable Hospital
Luton and Dunstable Hospital contributes to the training of Endoscopists and as a result has several trainees working in Endoscopy; this leaflet is provided to inform you about how this may affect your Endoscopy procedure, and support your decision as to whether you are happy to have a trainee perform the procedure.
Although the idea of a trainee may be unnerving it is often a very positive experience. All our Endoscopy trainees are in a structured training programme within the national guidelines.
Will they be supervised?
Under no circumstances are trainee Endoscopists unsupervised. Depending on the experience of the trainee, an experienced Consultant will be present, and supervising your Endoscopy procedure throughout or will be immediately available in the Endoscopy department. If at any time you or the trainee has any difficulties the trainer can intervene. All the Endoscopy trainers at Luton and Dunstable Hospital are accredited Endoscopy trainers and we regularly monitor their training skills.
Is it safe?
We carefully monitor our complication rates for Endoscopy and there is no difference in safety with a trainee Endoscopist.
Will it be more uncomfortable?
We carefully monitor patient comfort and have not found any suggestion it will be more uncomfortable.
Will it take longer?
While learning a trainee may be slower than an independent Endoscopist, however, our trainers are experienced in monitoring the length of a procedure and will take over if procedure seems prolonged. On a training list we allow a longer time for the whole Endoscopy experience, and patients often find this makes for a more relaxed atmosphere.
What should I do if I don’t want a trainee?
If you wish to let us know you are not happy to have a supervised trainee perform your procedure please inform us at least one week in advance of the procedure, so we can ensure you are not booked on a training list. The Endoscopy Booking Office can be contacted on 01582 497273.
What to look out for in the two weeks after the procedure
Contact the endoscopy unit on 01582 718486 (Monday to Friday, 8am to 6pm) or our 24 hour emergency advice line on 07815 178199 if you have any concerns or the following:
- Severe abdominal pain
- Vomiting
- Fever
- Passing a large amount of blood or blood clots from your back passage
